The Chain of Survival Steps
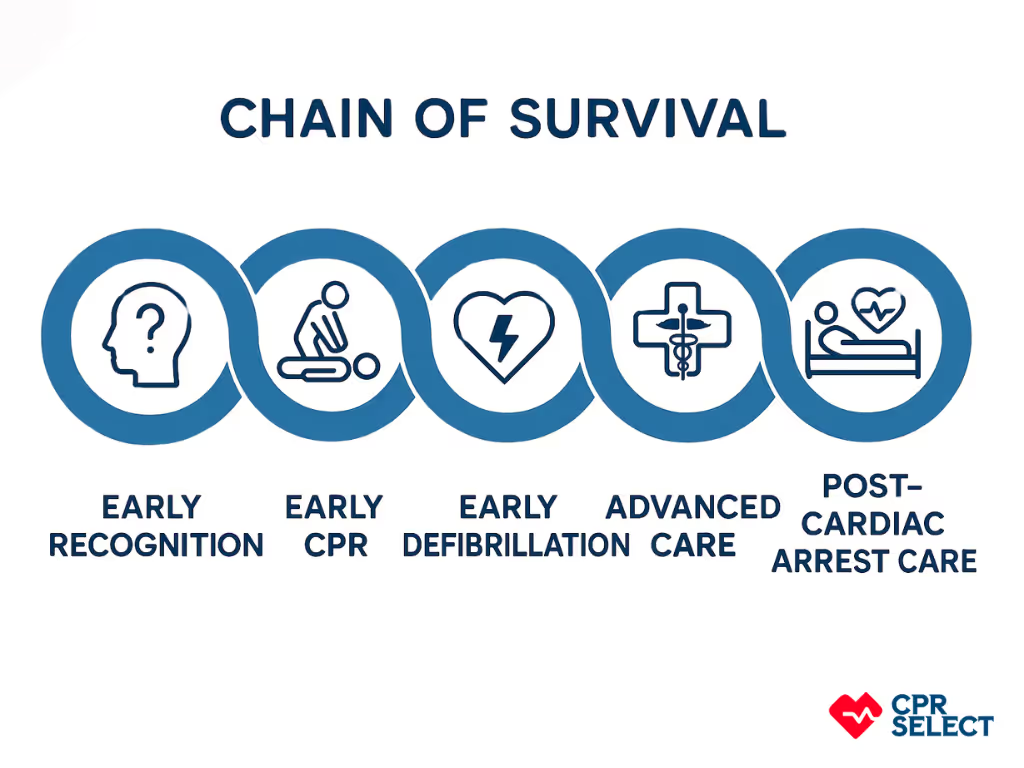
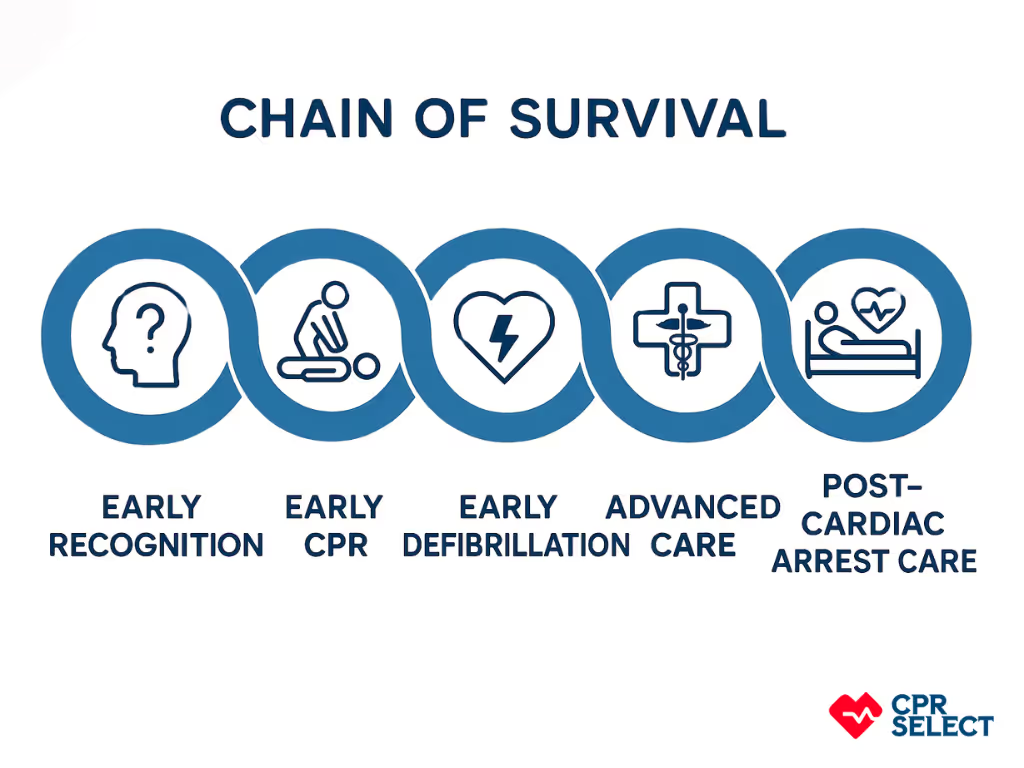
The 2025 AHA Guidelines introduce an updated Unified Chain of Survival, combining key steps for both in-hospital (IHCA) and out-of-hospital (OHCA) cardiac arrest. This unified approach streamlines critical actions to improve survival and recovery outcomes. The links include:
This update emphasizes continuous monitoring, feedback, and system-level improvements, reflecting the latest evidence to increase survival rates and quality of life after cardiac arrest.
The goal of an out-of-hospital cardiac arrest event is to restore a healthy heart rhythm and good neurological outcome. Bystanders can help save a cardiac arrest victim's life and improve patient outcomes by addressing the first three links in the AHA Chain of Survival. Action steps that bystanders can follow are explained below.


The foundational principle of the Chain of Survival is that delay in medical care after a cardiac arrest reduces survival chances. Each minute's delay drastically lowers the likelihood of survival, emphasizing the need for immediate and effective emergency response. Therefore, lay rescuers and emergency medical services must aim to have the fastest possible response. If you are on the scene, you must recognize the cardiac arrest as it occurs and ask another bystander to call 911 before taking any other rescue steps.
Many people, unfortunately, either ignore or misinterpret the critical signs of cardiac arrest, choosing to inform relatives over calling emergency services. This delay in seeking immediate medical help can significantly reduce the chances of survival in cardiac emergencies.

Starting CPR immediately can greatly increase survival chances after a cardiac arrest outside the hospital. If untrained, a bystander can perform Hands-only CPR or chest compressions-only CPR.
One of the most commonly held misconceptions about CPR is the idea that there must be at least two breaths between each compression. More than two breaths aren't much help. Therefore, it's much more important that public access defibrillation must be used as soon as possible.
Rescuers should start CPR immediately, with an emphasis on chest compression. Compressing the chest must be performed fast and hard enough.
According to the American Heart Association, the primary components of high-quality CPR are:

Early, rapid defibrillation is a critical link in the out-of-hospital chain of survival. It involves applying an automated external defibrillator (AED) to a person who is not breathing normally and whose heart rhythm is irregular. Public access defibrillation is used to restore normal heart rhythm and blood flow. If the heart stops beating, the AED delivers a powerful electric current through the chest wall to start the heart beating again, increasing the chances of survival. Defibrillation within 3–5 mins of collapse can produce a survival rate as high as 50–70%. So if public access defibrillation is available, rescuers must use it as soon as possible.

By this phase, medical professionals have taken over medical care, and advanced care will be provided. Advanced Life Support is a set of life-saving protocols and skills that extend Basic Life Support to further support circulation, airway, and adequate ventilation. Paramedics staff and other healthcare professionals are considered Advanced Life Support trained, including advanced scene management and medical care.
A medical professional must evaluate the cardiac patient for any potential cardiac problems like coronary artery diseases, which must be treated immediately. Therefore, the activation of emergency services comes before anything else.

Cardiac arrest survivors often face physical, cognitive, and psychological challenges after discharge from the hospital. They may require ongoing therapies and interventions, making aftercare a crucial component of the chain of survival to ensure lasting recovery. Referral to appropriate counseling or other support services, including primary care, should be assessed. Health professionals involved in resuscitation may also experience distress, and their organizations should provide proper support systems when needed.
For pediatric survivors, the 2025 AHA Guidelines emphasize follow-up: it is considered reasonable to evaluate physical, cognitive, and emotional needs within the first year after arrest, ensuring comprehensive care that addresses the child’s overall well-being.









According to the American Heart Association for Emergency Cardiovascular Care, accurate neurological prognostication in brain-injured cardiac arrest survivors is critical. This ensures that patient with significant potential for recovery is not destined for certain poor outcomes due to care withdrawal. This added step asks care teams to plan to investigate both the causes and the secondary effects of the out-of-hospital cardiac arrest event and ensure treatment continues.
The American Heart Association is committed to supporting research to update both in and out-of-hospital rescue guidelines. This means that the chain will likely improve in the next few years. The current basic life support guidelines still provide a strong outline for thinking about care and remind us that having knowledgeable certified rescuers is supremely important.

Cardiac arrest can strike both inside and outside the hospital, affecting hundreds of thousands of people annually in the United States. Brain injury begins within minutes due to lack of blood flow, and survival chances drop sharply after 10 minutes. However, timely and coordinated action can dramatically improve outcomes. This is where the Unified Chain of Survival comes in, integrating the critical steps for both out-of-hospital (OHCA) and in-hospital cardiac arrest (IHCA).
The Unified Chain of Survival emphasizes a seamless approach: early recognition of cardiac arrest, prompt activation of emergency response, high-quality CPR, rapid defibrillation, effective advanced life support, and comprehensive post-cardiac arrest care. The latest 2025 AHA updates highlight the importance of recovery, addressing the physical, cognitive, and emotional needs of survivors and their caregivers, including pediatric patients, within the first year after arrest.
By following this unified framework, bystanders, healthcare providers, and EMS teams can work together to maximize survival and long-term recovery for all cardiac arrest patients.
The history of the Chain of Survival is tied to the evolution of emergency medical services and the advancements in resuscitation techniques over the years. The concept of the Chain of Survival gained prominence in the late 20th century as medical professionals and researchers recognized the need to create a standardized framework for addressing sudden cardiac arrest and other life-threatening emergencies. One of the earliest mentions of this concept can be traced back to the American Heart Association (AHA), which played a significant role in promoting and disseminating guidelines for CPR and resuscitation techniques.
In the 1980s and 1990s, there was a growing emphasis on educating the public about basic CPR and the use of AEDs. Public awareness campaigns were launched to encourage bystanders to take immediate action when witnessing a cardiac arrest event. Furthermore, advancements in technology led to the development of more user-friendly AEDs that could be used by non-medical personnel.
Over time, various medical organizations, including the AHA, continued to refine the guidelines and protocols related to the Chain of Survival. These organizations advocated for improved training, public access to AEDs, and a greater focus on improving the quality of CPR and other life-saving interventions.
In recent years, advancements in telecommunication and mobile technology have also played a role in enhancing the Chain of Survival. Mobile apps and platforms that facilitate immediate communication with nearby CPR-trained individuals and dispatchers have emerged, enabling quicker response times and potentially saving more lives.
Out-of-hospital care is an important part of healthcare, as it allows patients to receive treatment in their homes or other settings where they feel comfortable. Survival rates of patients who receive out-of-hospital care can be influenced by a variety of factors, including:
The first three steps of the Chain must often be performed by bystanders, whether or not they know the cardiac arrest patient. Therefore, it's vital to that you recognize when cardiac arrest occurs and activate the Emergency Medical Services by calling 911.
But performing Cardiopulmonary Resuscitation and public access defibrillation as soon as possible is key to improving outcomes. According to 2014 statistics, about 45% of out-of-hospital cardiac arrest survivors received CPR from bystanders.
The American Heart Association updated the Chain of Survival in 2025 to reflect new evidence, streamline care, and improve patient outcomes across both out-of-hospital and in-hospital cardiac arrests. Key reasons for the update include:
By updating the Chain of Survival, the AHA aims to provide a more evidence-based, comprehensive framework that improves survival, recovery, and equity in cardiac arrest care.
Emergency medical personnel can improve survival rates for patients who require care outside of a hospital setting by providing prompt and appropriate treatment. This includes assessing the patient's condition, administering necessary medications, and initiating appropriate treatments. Additionally, emergency medical personnel must stay up-to-date on the latest protocols for out-of-hospital care and be prepared to respond quickly to any changes or complications that may arise.
A recent study in the Chain of Survival concept recommends strengthening the four links in the chain of survival according to the guidelines of the AHA Committee on Emergency Cardiac Care. These links include:
To enhance the survival rate of out-of-hospital patients, a range of treatments and interventions can be employed. These encompass fundamental life support measures like CPR and defibrillation, as well as the timely administration of prescribed medications. When required, initiating resuscitation is crucial. Moreover, post-discharge follow-up care plays a vital role in monitoring patients' recovery progress and mitigating potential complications. By employing a comprehensive approach that includes these interventions, healthcare professionals can significantly improve outcomes for individuals who experience medical emergencies outside of a hospital setting.
The most common causes of death for patients who do not receive timely out-of-hospital care include cardiac arrest, respiratory failure, stroke, and sepsis. Cardiac arrest is the most common cause of death in out-of-hospital settings, as it is often caused by a lack of oxygen to the heart or an irregular heart rhythm. Respiratory failure is another frequent cause of death in out-of-hospital settings, as it is often caused by a lack of oxygen to the lungs or an inability to breathe effectively. Stroke and sepsis are less common causes of death for out-of-hospital patients but can still result in serious complications and death.
Bystanders play a critical role in improving survival rates for patients who experience a medical emergency outside of a hospital setting. Bystanders should be trained in basic first aid and CPR, so they can respond quickly and appropriately when someone experiences a medical emergency. Bystanders should also call 911 immediately, as this is the best way to ensure that the patient receives timely and appropriate care. Additionally, bystanders can help support the patient until medical personnel arrives, providing comfort and reassurance.
The most effective treatment options for patients who require out-of-hospital care vary depending on the patient's individual needs and condition. Generally speaking. However, medical personnel should provide basic life support such as CPR, defibrillation, and oxygen if necessary. Medications may also be prescribed to alleviate symptoms or stabilize a patient’s condition in order to prevent further complications. Additionally, follow-up care is important for monitoring a patient’s recovery and preventing any further complications.
Emergency medical services can improve response times and increase the chances of survival for patients in need of out-of-hospital care by implementing various strategies. First, they can ensure that their personnel is well-trained and knowledgeable on the latest protocols for out-of-hospital care. Additionally, they can invest in rapid response vehicles and communication systems to enable them to respond quickly to medical emergencies. Finally, they can collaborate with local hospitals and other healthcare providers to ensure that the patient is able to receive timely and appropriate care in the event of a medical emergency.
Emergency medical personnel face various challenges when providing care outside of a hospital setting. One of the most significant challenges is the lack of access to diagnostic imaging and laboratory testing, which can make it difficult to diagnose and treat patients accurately. Additionally, many out-of-hospital settings do not have the same level of resources as a hospital, such as specialized equipment or medications. Furthermore, emergency medical personnel may also encounter environmental hazards or other challenges due to the location of the patient.
There are several resources available to help patients and their families prepare for medical emergencies that occur outside of a hospital setting. First, it is important for everyone to learn how to recognize the signs and symptoms of a medical emergency so they can take action quickly. Additionally, it is important for families to have a plan in place in case of an emergency, such as knowing who should be contacted and where to go for help. There are many first aid and CPR classes available that can provide individuals with the skills and knowledge needed to respond appropriately in an emergency situation.
Communities can support emergency medical personnel and improve survival rates for patients who require out-of-hospital care by providing them with the resources they need to respond quickly and effectively. This could include investing in rapid response vehicles, communication systems, specialized training, and other equipment necessary for responding to out-of-hospital emergencies. Additionally, communities can also provide financial support for emergency medical personnel, as well as educational opportunities for the public, in order to raise awareness about the importance of recognizing and responding to medical emergencies.
Public awareness and education are critical for improving the effectiveness of the Chain of Survival. Community-wide CPR training is essential, empowering individuals to provide immediate assistance until professional help arrives. Educating the public about the signs of cardiac arrest and the proper use of automated external defibrillators (AEDs) is equally important. Early recognition of cardiac arrest symptoms and prompt activation of emergency services can significantly impact outcomes. By fostering a well-informed and prepared community, the Chain of Survival can be strengthened, increasing the chances of successful interventions during emergencies.
According to the 2025 AHA updates, the Chain of Survival is now unified for adults, children, and infants. While anatomical and physiological differences still exist, the overall framework, including early recognition, activation of emergency response, high-quality CPR, defibrillation when indicated, advanced life support, and post-arrest care, is consistent across all age groups. This unified approach simplifies training, emphasizes early and high-quality interventions, and ensures that both lay rescuers and healthcare providers follow the same evidence-based steps to maximize survival and recovery outcomes for patients of any age.
The availability of medical technology and equipment is a major factor in the survival rates of out-of-hospital care patients. Access to sophisticated diagnostic tools, such as X-rays, CT scans, ultrasounds, and specialized treatments, can greatly improve the chances of survival for patients in need of emergency care. Additionally, access to advanced medical equipment such as ventilators, defibrillators, and other life-saving devices can also have a significant impact on the survival rates of out-of-hospital care patients.
Successful resuscitation requires quick and coordinated action by trained rescuers, each performing an important role. The chain of survival is an internationally recognized approach to resuscitation and summarizes the essential interventions to improve patient outcomes during medical emergencies. The chain of survival applies to all OHCAs in adults, children, and infants. Early recognition of OHCA, immediate CPR, and early defibrillation remain the key to improving outcomes. The evidence for high-quality post-resuscitation care continues to evolve to improve results further.
Sources: