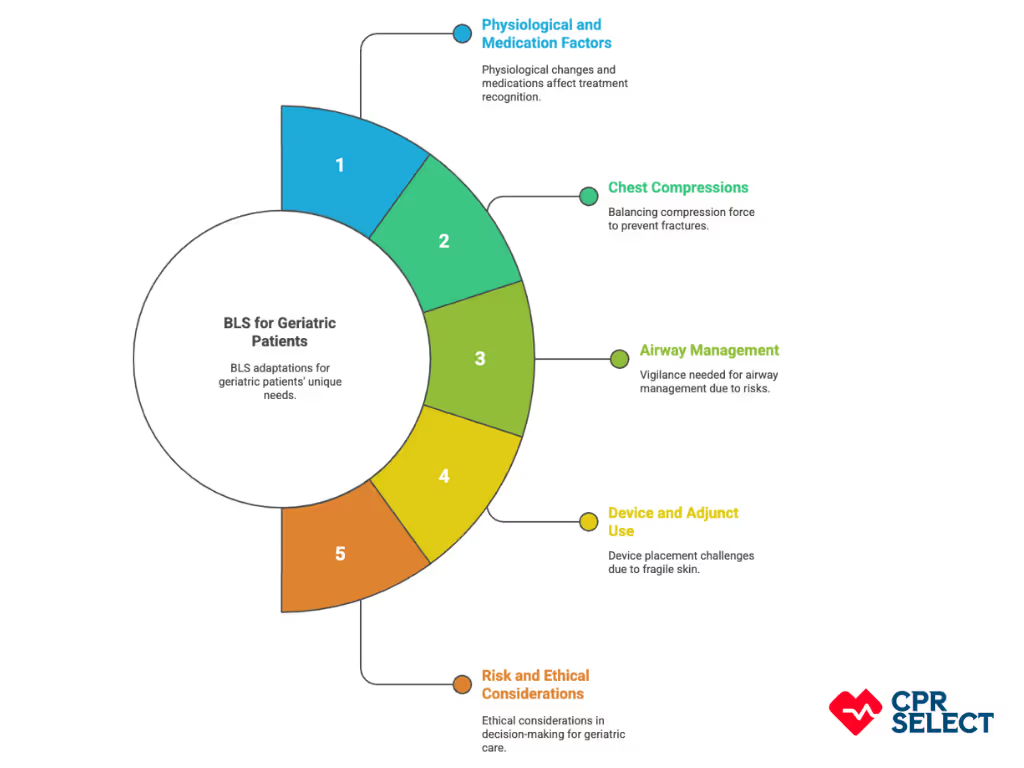
Basic Life Support (BLS) for geriatric patients requires special attention because older adults often have frailty, chronic conditions, and higher risks during resuscitation. Standard BLS techniques must be adapted to their unique needs to ensure safety and effectiveness.
This article explains how BLS is modified for elderly patients, the challenges caregivers and healthcare providers face, and why proper training is essential. It also highlights the role of online BLS certification in equipping individuals with the right skills to respond confidently in emergencies involving older adults.
Tailoring BLS to geriatric care, caregivers, and responders can improve survival chances, reduce complications, and provide care that respects both safety and patient goals.
Why Is BLS Important in Elderly Care?
Basic Life Support (BLS) is critical in elderly care because quick CPR, ventilation, and defibrillation can mean the difference between life and death. For older adults, every second counts as delays quickly reduce survival rates and increase the risk of brain injury or permanent decline.
Age brings unique challenges
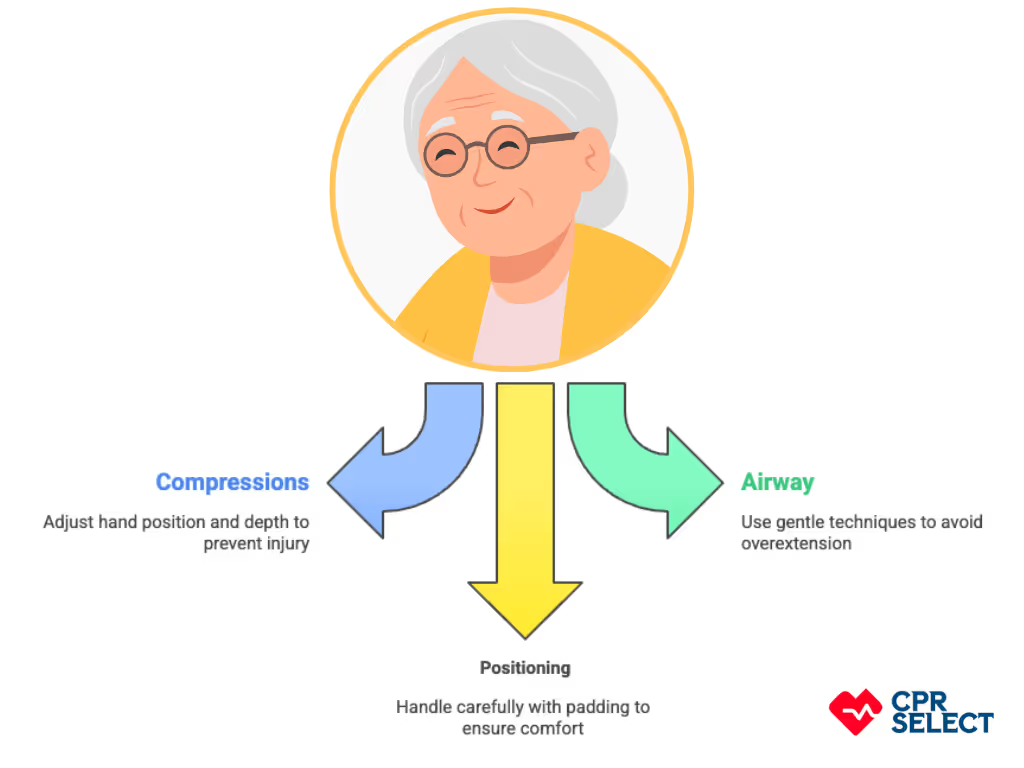
Weaker heart and lung function, stiffer chest walls, and higher risks of cardiac arrest or fainting. These vulnerabilities make immediate BLS even more important, especially in settings like nursing homes, assisted living facilities, or when seniors live alone.
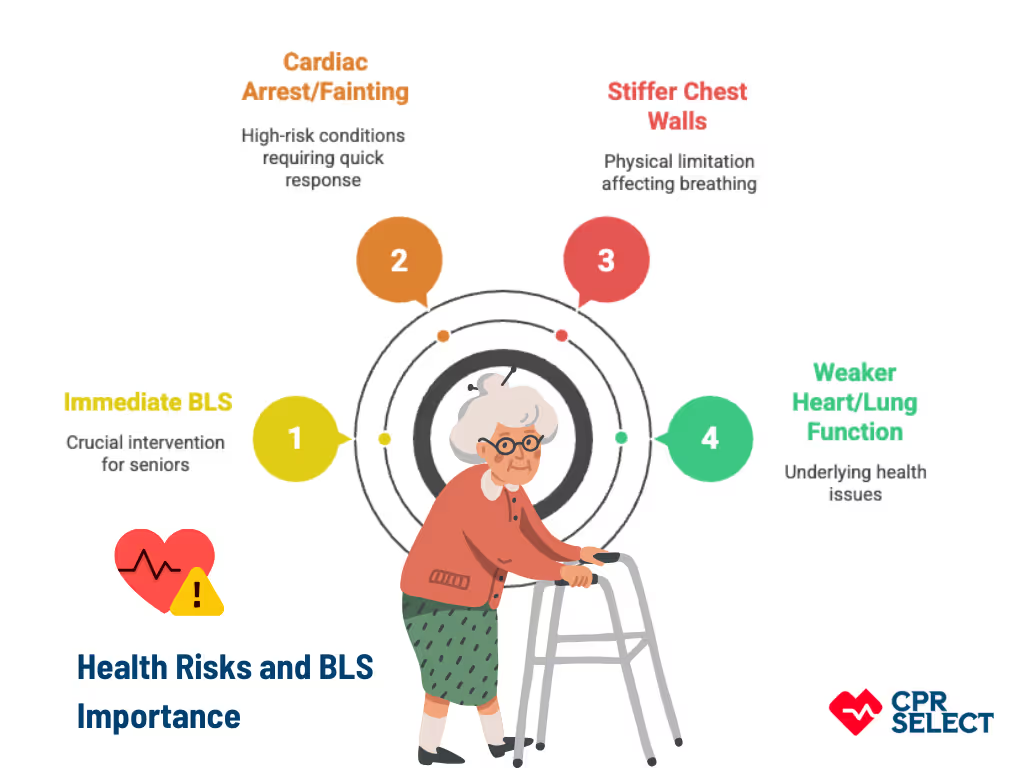
With prompt action, BLS improves the chances of restoring circulation, protecting the brain, and helping patients return home instead of long term care. That’s why caregivers, healthcare workers, and family members all need to understand its importance. Enrolling in ATAC’s online BLS certification ensures you have the right training and confidence to respond when it matters most.
What Factors Influence Outcomes?
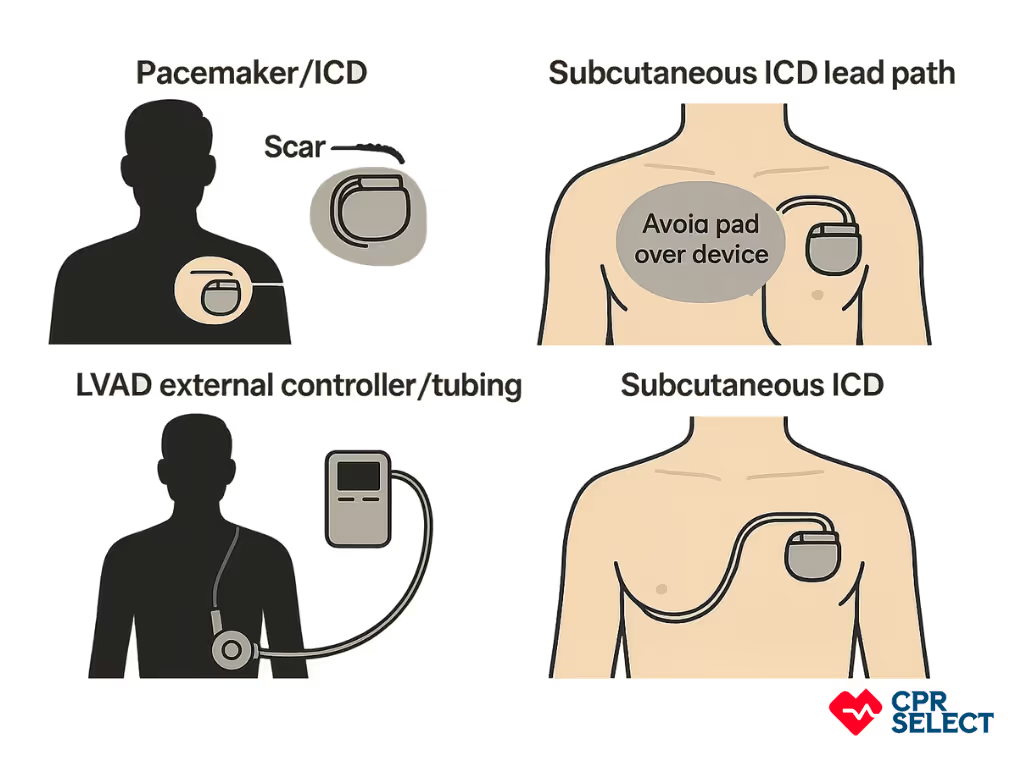
The effectiveness of BLS in elderly patients depends on the care setting, comorbidities, and available resources. For example, longer EMS response times at home can limit survival, while access to AEDs in nursing facilities shortens time to defibrillation. Advance directives and do not resuscitate orders also guide whether BLS should be initiated. ATAC’s online BLS certification helps caregivers and healthcare providers prepare for these real world challenges by teaching practical skills, scenario based responses, and decision making strategies that align with patient needs.
What Common Age Related Health Risks Requiring BLS?
Older adults face a higher chance of sudden, life threatening events due to multiple age related conditions. These include cardiac, respiratory, neurological, traumatic, metabolic, and device related emergencies that often demand immediate BLS.
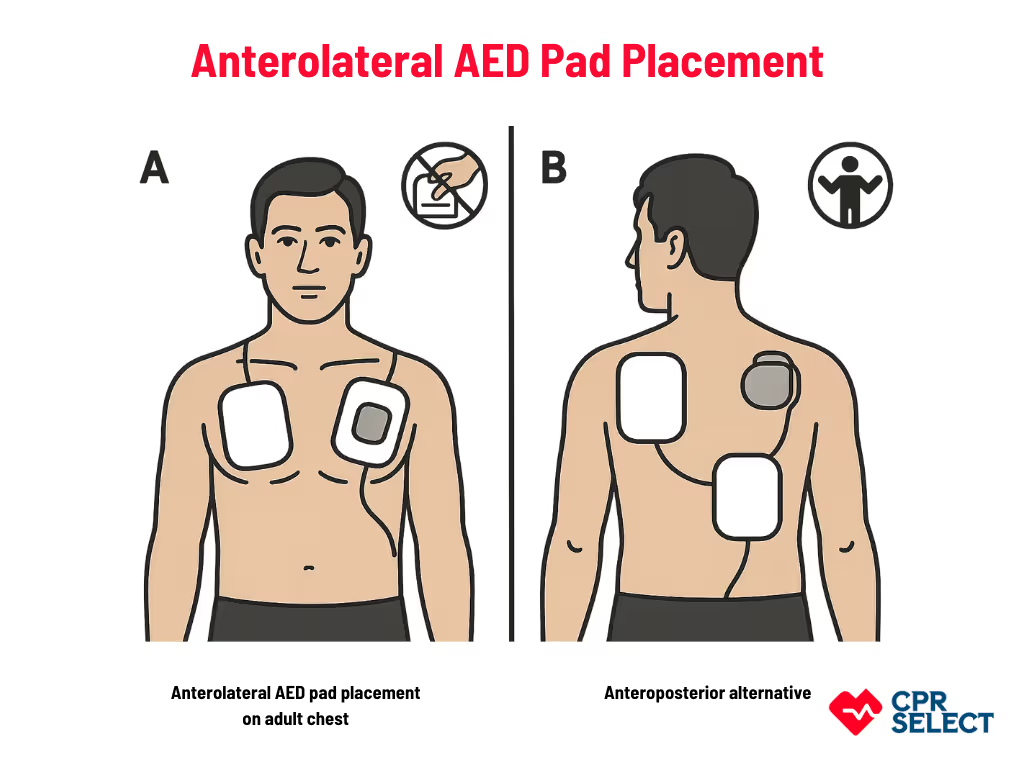
- Cardiac conditions (arrhythmias, coronary artery disease): Arrhythmias, heart attacks, or coronary artery disease can quickly lead to cardiac arrest. High quality compressions (5–6 cm deep, 100–120 per minute) and early defibrillation with an AED are the top priorities.
- Respiratory failure and chronic lung disease (COPD, fibrosis): Breathing problems from chronic lung disease or acute exacerbations may cause collapse. If the patient has a pulse but isn’t breathing, provide rescue breaths every 5–6 seconds. For presumed respiratory arrest, follow 30 compressions and 2 breaths per cycle.
- Neurological events (stroke, seizures): Stroke or seizures can cause sudden loss of consciousness or breathing problems. Protect seizure patients from injury, clear the airway once movements stop, and check for breathing and a pulse. Start CPR if necessary.
- Falls and trauma (hip fractures, head injuries): Even ground level falls can cause brain injuries, airway compromise, or major bleeding. Control bleeding with direct pressure or a tourniquet, protect the spine, and ensure airway and breathing while waiting for advanced help.
- Metabolic, endocrine, and toxic states (hypoglycemia, overdose): Low blood sugar, electrolyte imbalance, or medication overdose may lead to unresponsiveness. Provide supportive ventilation and circulation care until medical treatment is available. Do not give oral glucose if the patient is unresponsive.
- Device and procedure complications (pacemakers, grafts): Implants or recent surgeries may cause sudden deterioration. Continue CPR if the patient is pulseless and unresponsive, and use an AED without placing pads directly over implanted devices.
These six categories highlight why older adults are more likely to need BLS. Recognizing these risks early and responding quickly is key to improving outcomes. Since cardiac events are the most time sensitive, the next section will focus on the signs of cardiac arrest in elderly patients.
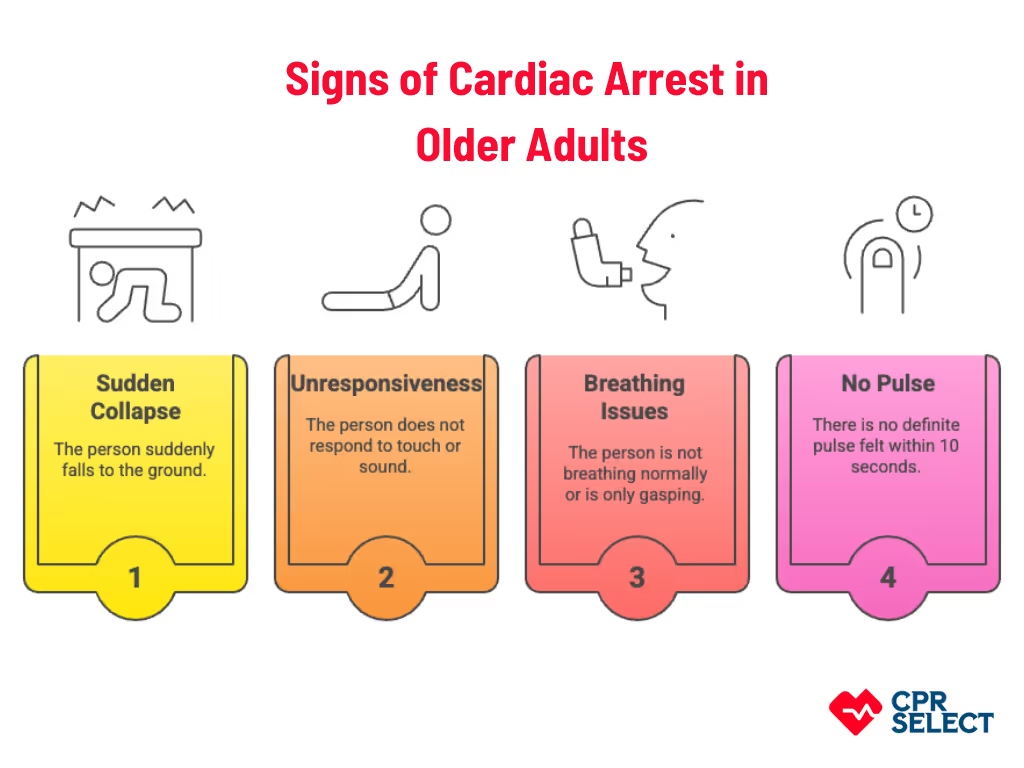
What Are the Signs of Cardiac Arrest in Older Adults?
Cardiac arrest in older adults usually shows up as:
- Sudden collapse
- Unresponsiveness
- No normal breathing or only gasping
- No definite pulse within 10 seconds
Other cues may include a limp body, agonal gasps, or abrupt loss of responsiveness. Chronic conditions or medications can make recognition tricky, but when in doubt, treat it as cardiac arrest.
What Should Rescuers Do?
To act quickly and effectively, rescuers should follow these simple steps:
- Shake and call the person to check responsiveness
- Look for chest rise and listen for breathing (no more than 10 seconds)
- Begin chest compressions at 100–120 per minute, at least 5 cm deep, if no normal breathing is found
Recognizing cardiac arrest in older adults depends on spotting the core signs and acting even when comorbidities create confusing cues. Quick identification is what drives immediate basic life support.