Neonatal resuscitation is a critical skill that supports a newborn’s breathing and circulation when they struggle at birth. Quick, competent action prevents brain injury and saves lives. Through structured training and practice, providers gain the skills to respond effectively. CPR Select’s Basic Life Support certification offers a recognized pathway to build this lifesaving competency.
This article will cover causes of neonatal compromise, clinical signs, stepwise procedures, equipment, common errors, care for special populations, certification pathways, post resuscitation monitoring, and frequently asked questions. It will not provide detailed pharmacology or individualized medical orders requiring specialist consultation.
Understanding Neonatal Resuscitation
Neonatal resuscitation is a set of immediate actions to restore breathing and circulation in a newborn. It is critical in the first moments after birth because timely oxygen delivery prevents organ injury and supports the transition to independent breathing. Key steps include the following
- Airway assessment with neutral head and neck positioning
- Positive pressure ventilation at 40–60 breaths per minute when indicated
- Chest compressions at a 3:1 ratio if the heart rate stays below 60, and medications such as epinephrine if bradycardia persists.
These interventions, performed by trained professionals, aim to restore gas exchange and blood flow.
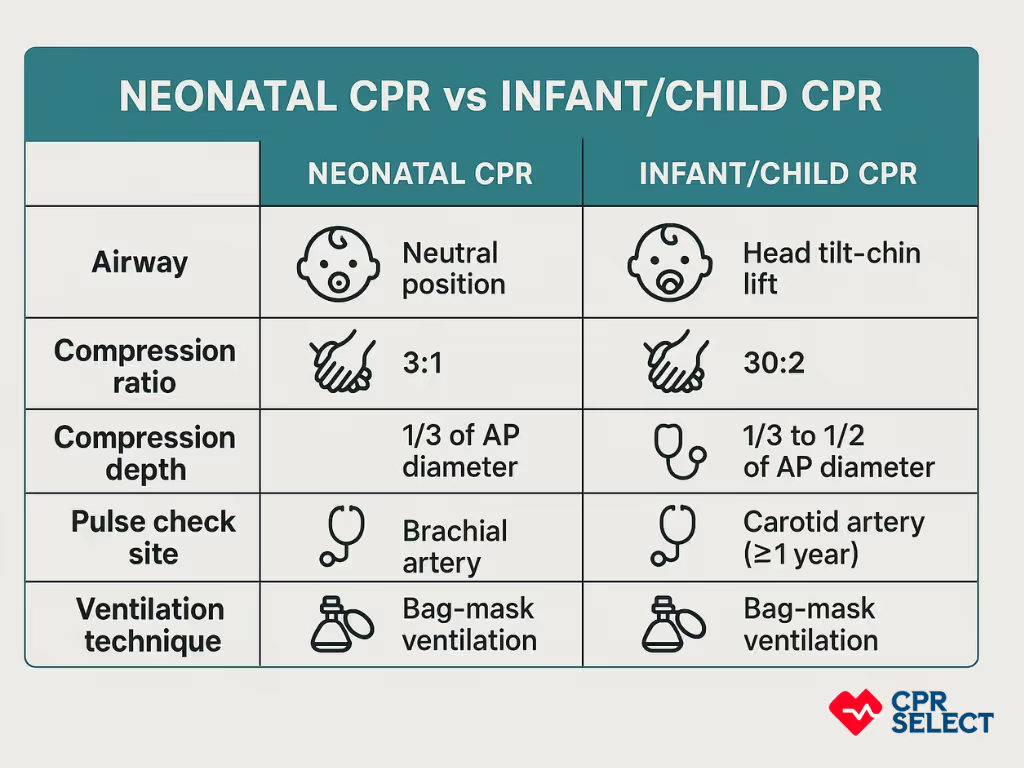
How does cardiopulmonary resuscitation differ in newborns compared to older infants?
Cardiopulmonary resuscitation in newborns emphasizes gentle ventilation, maintaining airway patency, and rapid assessment of heart rate rather than immediate strong chest compressions. In older infants, rescuers follow Child & Baby CPR steps with proper compression depth, brachial pulse checks, and compressions with breaths at the correct compression ratio.
Why Is Timing Critical in Neonatal Resuscitation?
Timing is critical in neonatal resuscitation because the main focus is correcting inadequate ventilation and supporting circulation until the infant can breathe and stabilize on their own. Initial assessment looks at muscle tone, breathing or crying, and heart rate. A heart rate under 100 calls for ventilation; under 60 requires compressions and possibly medication.
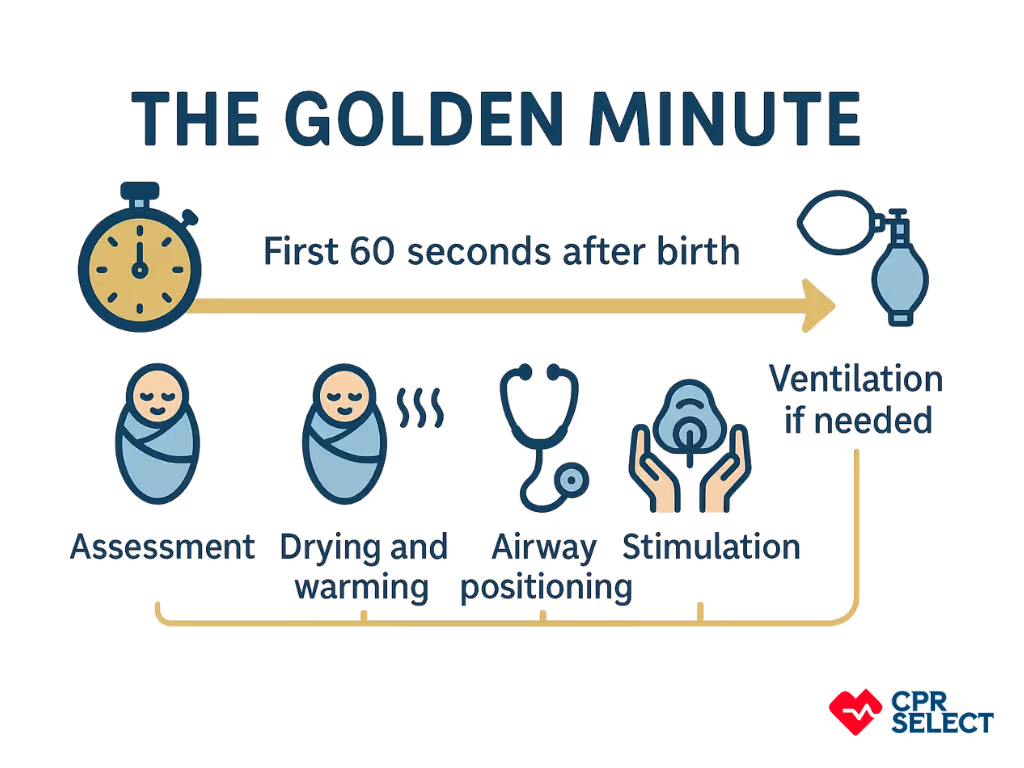
Resuscitation must happen quickly. Guidelines call for assessment within seconds of delivery and, when needed, ventilation within the first minute or the “golden minute.” Prompt action greatly reduces the risk of brain injury and long term complications.
When is Neonatal Resuscitation Needed?
Resuscitation may be needed in delivery rooms, operating theaters, neonatal intensive care units, emergency transport, or resource-limited settings. High risk deliveries, such as those with prematurity or fetal distress, require extra preparation. Essential equipment includes a resuscitation table, neonatal bag mask devices, oxygen, suction, pulse oximeter, ECG leads, intubation tools, and vascular access supplies.
Success depends on trained teams, proper equipment, and clear protocols. Regular training, checklists, and post event debriefings improve performance and adherence to guidelines.
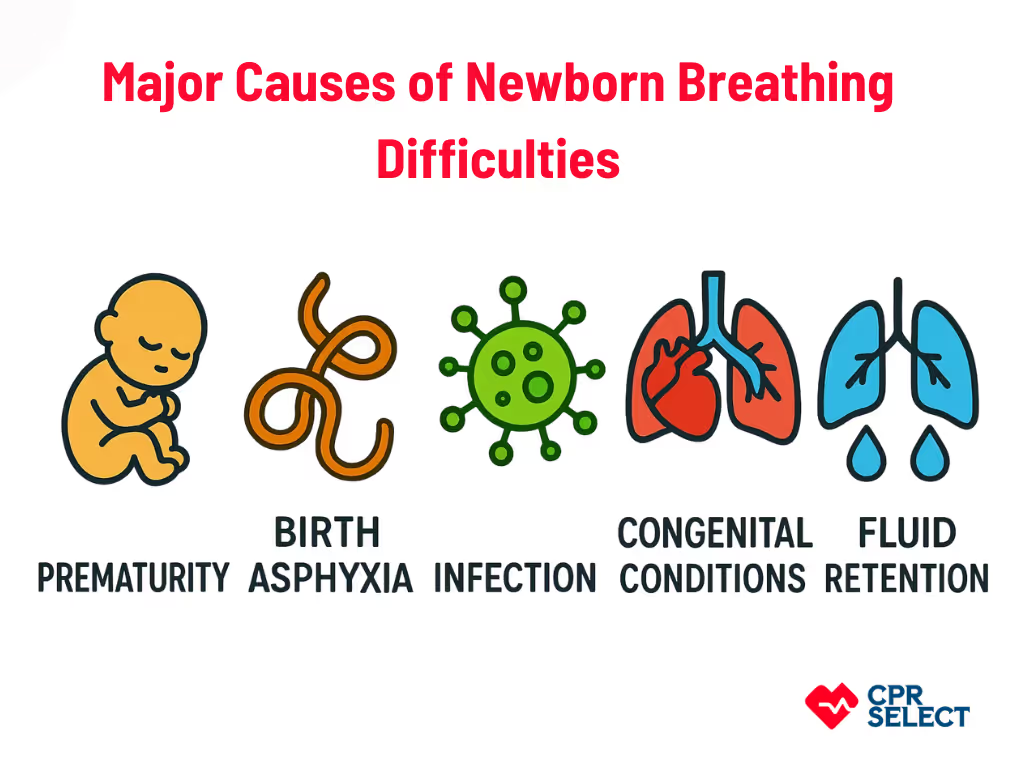
What Causes Newborn Breathing Difficulties?
Newborn breathing problems can come from several causes. Identifying the source helps guide resuscitation and care.
- Prematurity: Underdeveloped lungs, lack of surfactant, and weak respiratory drive increase the risk of respiratory distress syndrome. May require CPAP, surfactant therapy, and thermal or glucose management.
- Birth Asphyxia: Lack of oxygen during birth can depress breathing centers and impair lung function. Requires rapid airway support, ventilation, and possibly advanced resuscitation.
- Infections: Conditions like chorioamnionitis or sepsis trigger inflammation and respiratory distress. Supportive care and early antibiotics are critical.
- Congenital Conditions: Structural issues such as choanal atresia, diaphragmatic hernia, or heart malformations obstruct breathing and circulation, often needing specialized care.
- Transient Adaptation Issues: Retained lung fluid or delayed aeration may cause temporary distress. Usually improves with stimulation, airway clearance, or short term ventilation.
- Airway Obstruction: Secretions, poor tone, or anatomical blockages can block airflow. Managed with positioning, suctioning, and basic airway maneuvers; advanced airways if needed.
- Metabolic and Systemic Causes: Hypoglycemia, hypothermia, or electrolyte problems suppress breathing. Requires correction of underlying issues with supportive care.
- Cardiac Causes: Heart defects or duct dependent lesions impair oxygen delivery, often presenting with cyanosis unresponsive to oxygen. Needs urgent cardiac evaluation and transfer.
Recognizing these causes helps providers choose the right interventions and stabilize newborns effectively.
Signs a Newborn Needs Resuscitation
A newborn needs resuscitation when there is weak or absent breathing, bluish skin, or a heart rate below 100 beats per minute. These core signs help clinicians decide when to act.
Primary Warning Signs
- Weak or no breathing: Absence of respirations causes rapid hypoxia and signals urgent support.
- Bluish skin (central cyanosis): Discoloration of the trunk or mucous membranes indicates poor oxygenation.
- Low heart rate (<100 bpm): Measured by auscultation, pulse oximetry, or ECG, it shows cardiovascular compromise.
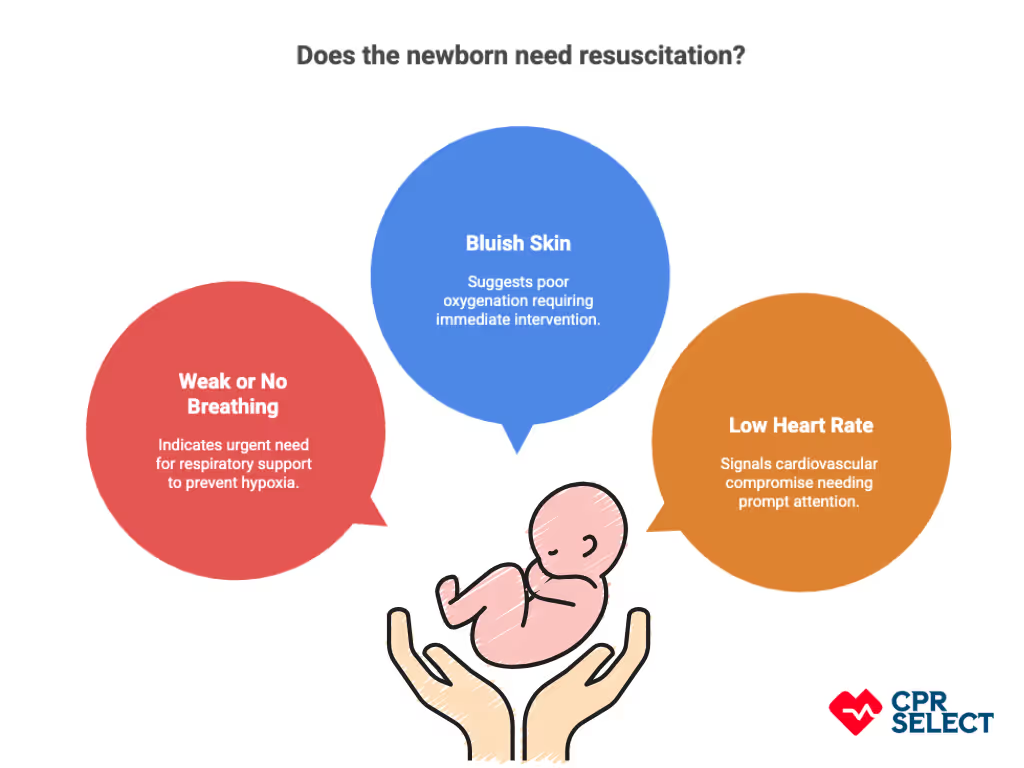
Secondary Signs
- Poor muscle tone: Limp posture often accompanies respiratory failure.
- Ineffective effort: Gasping or shallow breaths may progress to apnea.
- Other changes: Weak cry, apnea episodes, or falling oxygen saturation strengthen the need for resuscitation.
When Should Neonatal Resuscitation Begin?
Neonatal resuscitation should begin within the first minute after birth if the newborn shows no effective breathing or has a low heart rate. This “golden minute” is critical because early action can prevent brain injury and long term complications. Resuscitation may also be required later if the baby develops progressive cyanosis or breathing distress after initial transition. Certain high risk factors, such as prematurity, meconium-stained fluid, or an emergency C-section, make resuscitation more likely.
What Immediate Actions Should Be Taken?
Once signs of distress are recognized, the first step is to call for skilled help. The newborn’s head should be placed in a neutral position to keep the airway open. Equipment such as a bag mask, suction, pulse oximeter, and warm linens should be prepared immediately. The infant must be kept warm and dry, either under a blanket or a radiant heater, to prevent heat loss while resuscitation steps are carried out.



