Animal bites can cause serious injuries if not treated promptly. This article explains why immediate first aid and proper wound care matter and highlights the health risks that make quick action essential.
It covers bites from mammals (such as dogs, cats, and bats), reptiles (such as snakes), and arthropods (such as spiders and scorpions). You’ll learn how to recognize danger signs, provide immediate first aid, know when to seek medical care, and reduce the risk of infection or other complications.
What is an Animal Bite?
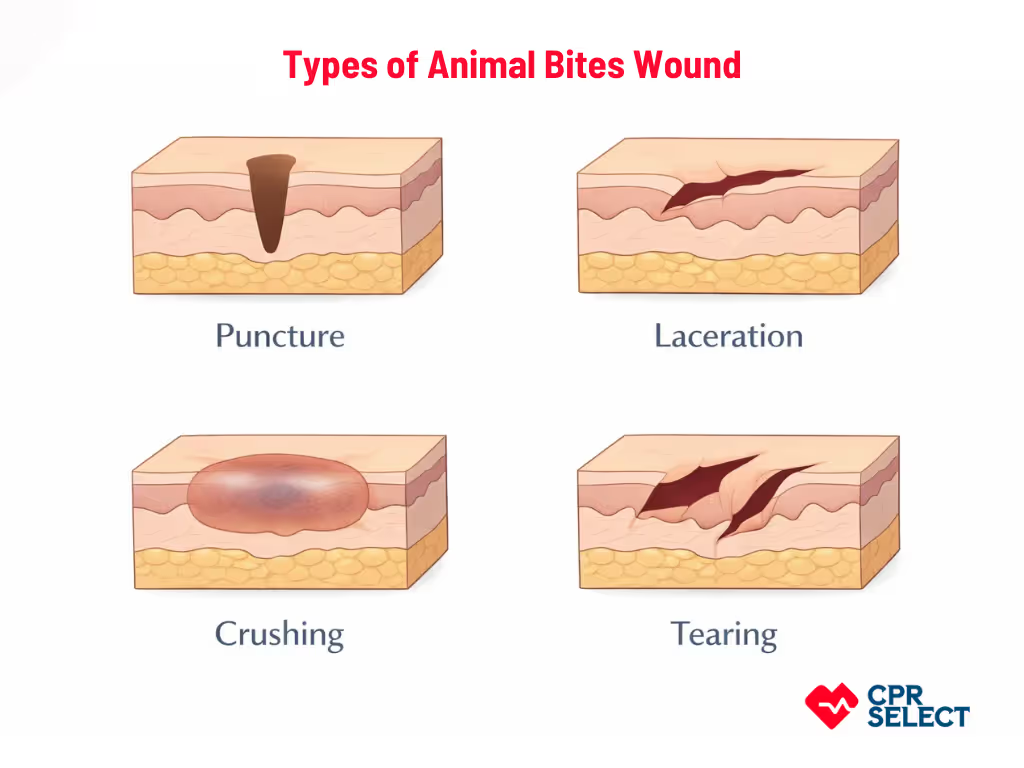
An animal bite is an injury that occurs when an animal’s teeth or claws break or tear the skin. Unlike other skin injuries, animal bites carry a higher risk of infection and require specific first aid and medical evaluation. Animal bites can cause different types of wounds:
- Puncture wounds drive bacteria deep into tissue.
- Lacerations create irregular tears that may need careful cleaning or closure.
- Crushing injuries damage deeper tissue and may involve bones or muscles.
- Tearing injuries remove soft tissue and can require advanced medical care.
The type of wound affects infection risk and treatment decisions.
An animal bite specifically involves skin penetration or tearing. Superficial scratches or simple contact without broken skin are not considered animal bites. Understanding what qualifies as an animal bite helps ensure proper first aid and timely medical response, which the next section explores in more detail.
What are the Types of Animal Bites?
Animal bites are grouped based on the type of animal, the setting where the bite occurs, and how the injury happens.
- Domestic (such as dogs and cats),
- Wild such as raccoons and bats), and
- venomous (such as snakes or cone snails).
Each category carries different risks, including infection, rabies exposure, or toxin effects, which influence how urgently medical care is needed.
1. Domestic Animal Bites
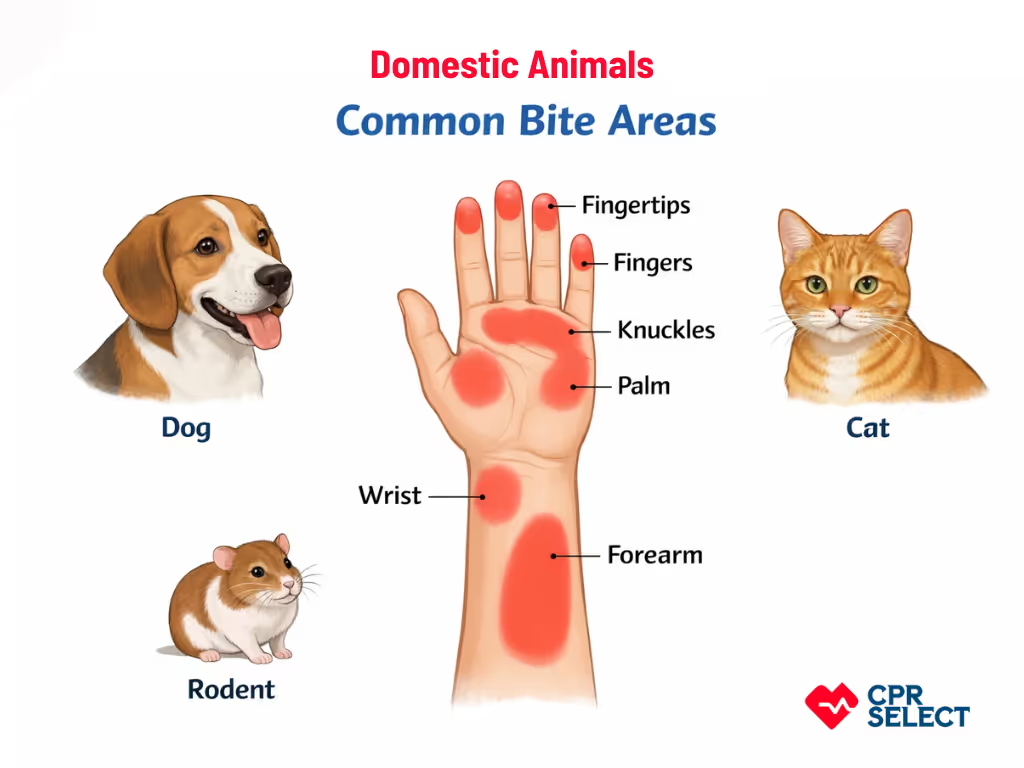
Domestic animal bites come from household pets such as dogs, cats, and rodents. These bites often cause crushing injuries, lacerations, or deep puncture wounds, which can trap bacteria and debris, increasing infection risk.
- Dogs: Dog bites produce crushing injuries, lacerations, or tissue avulsions. These wounds can damage underlying structures like tendons or nerves and have a higher risk of infection due to tissue devitalization.
- Cats: Cat bites usually create deep, narrow punctures that can trap saliva and debris, making infection more likely. Pasteurella multocida is a common pathogen in cat bite infections.
- Pet rodents: Rodent bites cause small punctures or minor tears and can transmit bacteria such as Streptobacillus moniliformis. Even small wounds on hands or face can lead to infection if untreated.
Infection risk factors include bite location (hands, face, joints), wound depth, delayed cleaning, and patient conditions like diabetes or immunosuppression. These increase the likelihood of complications such as cellulitis, septic arthritis, or osteomyelitis.
First Aid Treatment for Domestic Animal Bites
Immediately irrigate the wound with clean water or saline, apply pressure to control bleeding, cover with a sterile dressing, and seek medical care for deep, facial, or hand wounds, or bites from cats or rodents. Ensure tetanus status is up to date, and consult a clinician for possible antibiotics or rabies assessment if the animal’s vaccination status is unknown.
Domestic animal bites involve household pets with characteristic wound patterns and shared infection risks. The next section covers wild animal bites, which present different exposure contexts and pathogen risks.
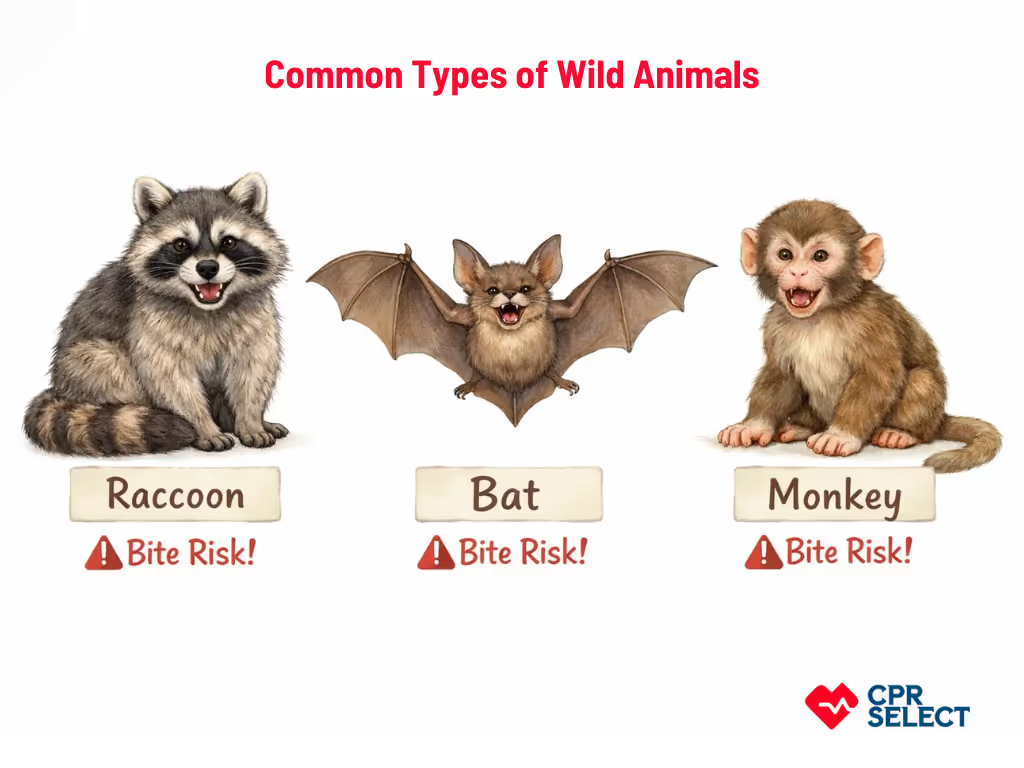
2. Wild Animal Bites
Wild animal bites are injuries from free-living wildlife such as raccoons, bats, foxes, monkeys, and deer. These bites are unpredictable and carry higher risks of zoonotic infections like rabies, leptospirosis, tetanus, and other bacterial infections. Wounds often involve deep punctures and environmental contamination, making prompt first aid essential, including thorough irrigation, tetanus status review, and consideration of rabies postexposure prophylaxis. Specific species pose unique risks:
- Raccoons can carry rabies virus variants
- Bats can transmit rabies even without visible wounds
- Monkeys may transmit herpes B virus or simian B virus during captive or tourist encounters.
First Aid Treatment for Wild Animal Bites
Clean the wound with water for at least five minutes, control bleeding, cover with a sterile dressing, and seek urgent medical evaluation, especially for deep punctures or high-risk species. Preventive measures include avoiding wildlife, securing attractants, and reporting aggressive animals to local authorities.
3. Venomous Animal Bites
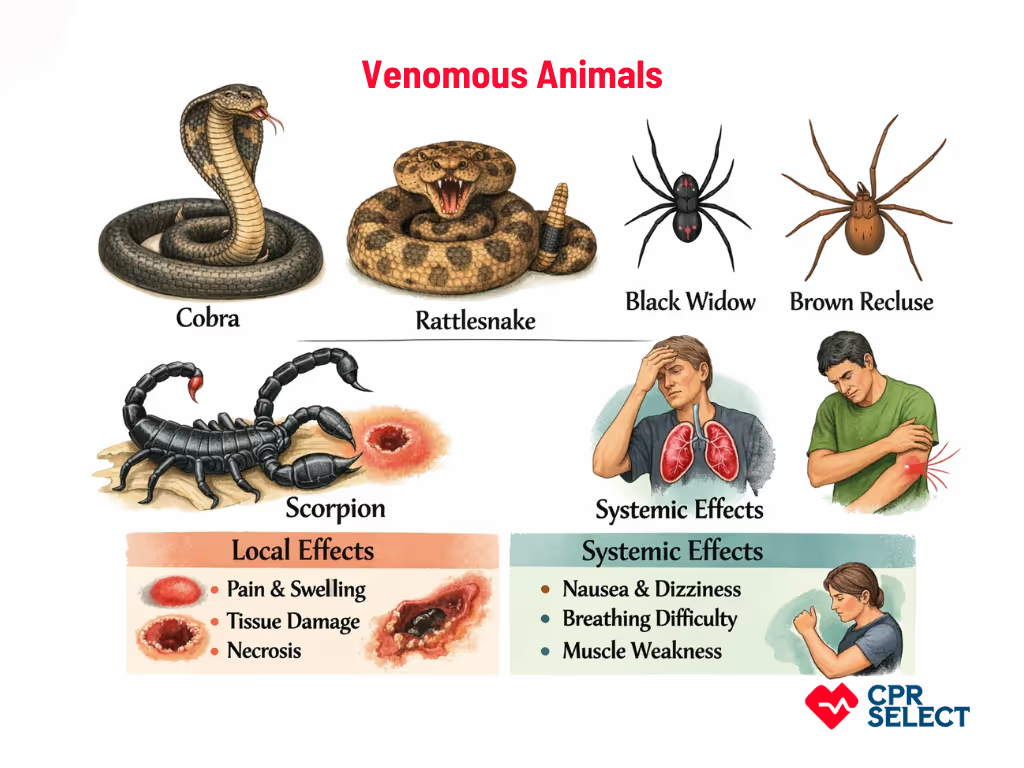
A venomous animal bite occurs when an animal injects venom into human tissue or the bloodstream, causing local tissue damage and potentially serious systemic effects. Unlike nonvenomous bites, these require prompt medical attention and careful risk assessment.
Venomous bites are typically classified by animal type: snakes (e.g., cobras, rattlesnakes), spiders (e.g., black widows, brown recluses), and scorpions (e.g., Leiurus, Centruroides). Snake bites are often further categorized as viper (causing coagulopathy and tissue necrosis) or elapid (causing neurotoxicity) envenomations.
Venom effects are either local (pain, swelling, bruising, or tissue necrosis) or systemic (neurotoxic symptoms, blood clotting problems, or cardiovascular instability). Immediate concerns include rapid tissue injury, allergic reactions like anaphylaxis, and signs of organ involvement, all of which require urgent medical evaluation and possibly antivenom.
First Aid for Venomous Animal Bites
If bitten by a venomous animal, seek emergency medical care immediately. Move away from the animal and keep the person calm and still to slow venom spread. Gently clean the wound with soap and water. Do not cut, suck, or apply ice. Keep the affected limb immobilized and at or below heart level. Avoid tourniquets or other harmful interventions. In some regions, pressure immobilization bandages may be recommended for specific bites, but only if applied correctly. The priority is stabilization and rapid transport for professional treatment, including possible antivenom.
Rapid medical evaluation is essential. Local tissue effects and systemic symptoms can progress quickly, and professional treatment, including antivenom and supportive care, is often required.
Other Special-Case Bites
Special-case bites include injuries from rodents or humans. These bites are associated with unique infection risks, such as rat-bite fever or serious bacterial infections from human bites. Because of their high complication rates, these bites always require careful medical assessment.



.avif)
