What CPR Select Recommends to Prevent Diabetic Emergencies
At CPR Select, we emphasize that preventing diabetic emergencies begins with consistent daily habits and proactive care. The goal is to lower the chance of sudden complications while improving overall safety and well being.
1. Lifestyle Management
Follow a balanced meal plan aligned with your medication, exercise regularly (150 minutes of moderate activity weekly plus strength training), limit alcohol, and manage stress and sleep. These habits help keep blood sugar stable.
2. Medication Adherence
Take insulin or other diabetes medications exactly as prescribed. Double check doses, store insulin properly, and always keep supplies on hand. Missed or incorrect doses are a leading cause of emergencies, so consistency is key.
3. Regular Monitoring
Check blood glucose at recommended times: before meals, at bedtime, when feeling unwell, and after activity. Use ketone testing when glucose runs high. Track patterns, not just single readings, to make better decisions.
4. Education and Preparedness
Carry a written emergency plan, keep glucagon and quick sugar sources accessible, and make sure caregivers know how to use them. Practice emergency responses so you feel confident if a crisis occurs.
5. Ongoing Healthcare Support
Stay in regular contact with your healthcare team for medication reviews, checkups, and complication screening. Access to supplies and follow up care reinforces your prevention routine.
Prevention works best when these strategies are combined and personalized. CPR Select also recommends that patients and caregivers complete first aid and emergency training so they are ready to respond quickly if an emergency does happen.
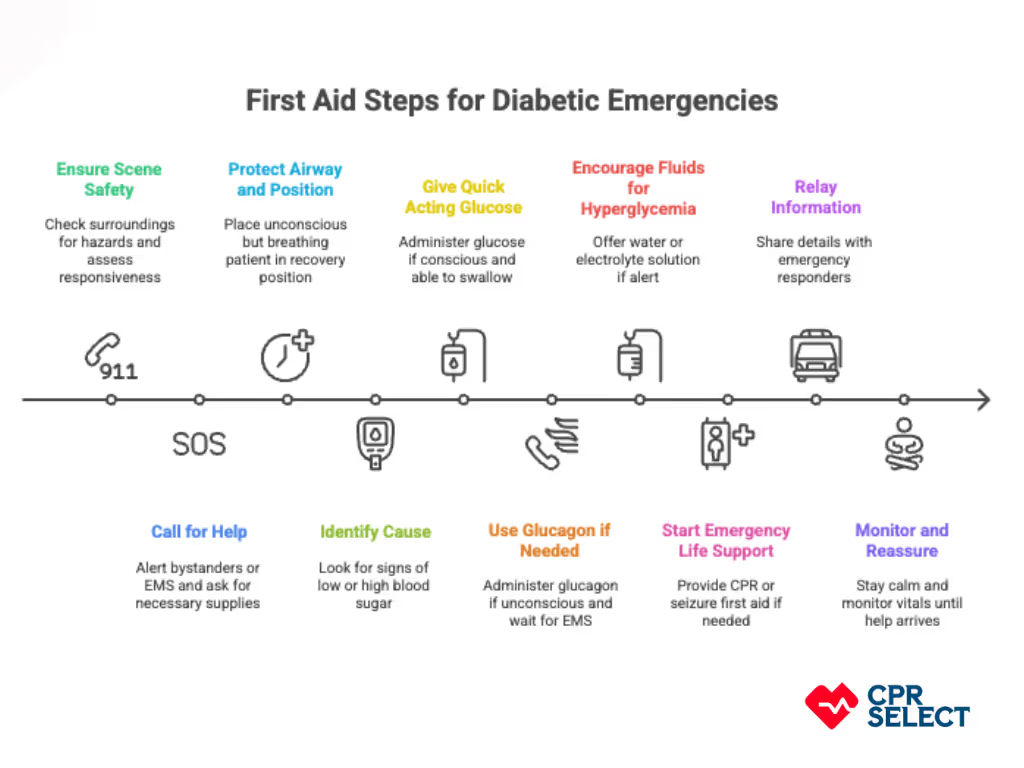
What is the Role of First Aid Training in Managing Diabetic Emergencies
First aid training prepares people to recognize and respond to diabetic emergencies quickly and safely. It teaches practical skills like glucose checks, safe glucose administration, and airway protection, as well as decision making on when to call EMS. Training also builds teamwork, communication, and readiness for worst case scenarios, often alongside CPR and BLS. Regular certification and refreshers keep skills sharp, turning bystanders into confident, effective first responders.
Frequently Asked Questions (FAQs)
Here are the most common concerns about diabetic emergencies.
What should you not do during a diabetic emergency?
Do not force food or drink into the mouth of someone who has impaired consciousness. This can cause choking. Do not give insulin or glucose without confirming blood glucose levels, as incorrect dosing can worsen the condition. Never leave the patient alone, since seizures or loss of airway can happen quickly.
Can you give food or drink to an unconscious diabetic?
No. Giving anything by mouth to an unconscious person risks aspiration. Instead, place the patient in the recovery position, open the airway, and call emergency services immediately.
When should you call emergency services?
Call immediately if the person is unresponsive, has seizures lasting longer than five minutes, shows signs of respiratory distress, persistent vomiting, recurrent loss of consciousness, or blood glucose <50 mg/dL (2.8 mmol/L) that does not improve with treatment. Also call for symptoms of diabetic ketoacidosis (deep rapid breathing, fruity breath odor) or blood glucose >300 mg/dL (16.7 mmol/L) with dehydration.
How often should blood sugar be checked during an acute episode?
During hypoglycemia treatment, recheck every 15 minutes until blood glucose is stable above 72 mg/dL (4.0 mmol/L). For unstable hyperglycemia, check every 30–60 minutes until levels improve.
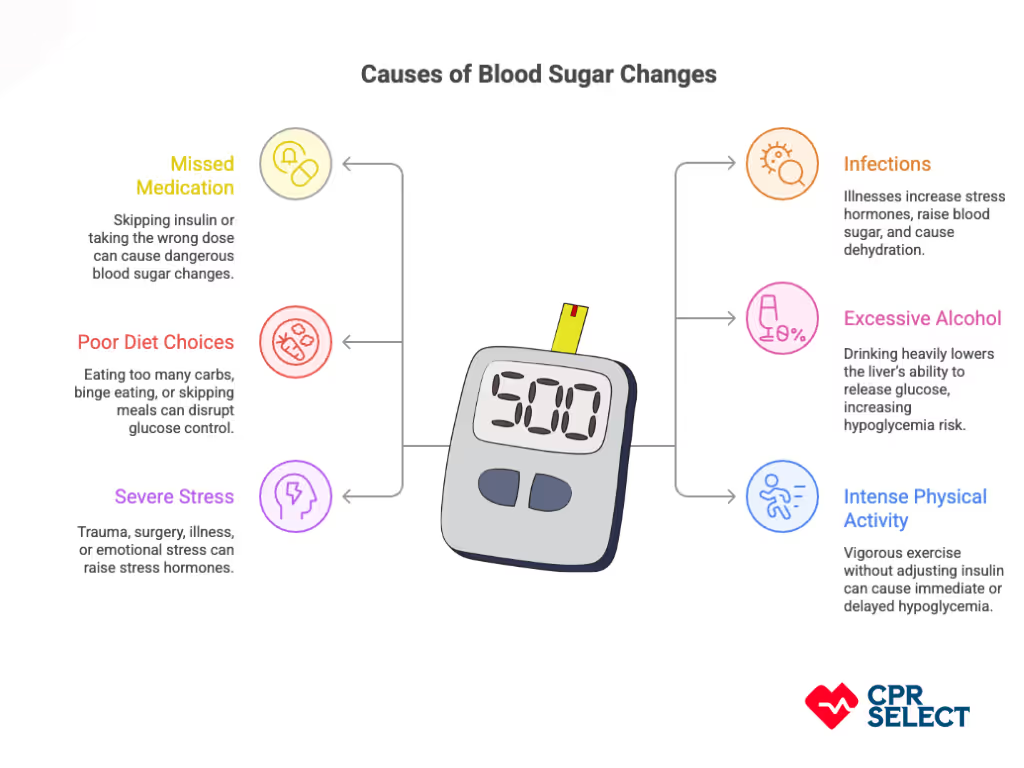
What are common triggers of diabetic emergencies?
Triggers include missed or excess insulin, other medication errors, fasting, heavy alcohol use, infections (e.g., flu, UTIs), trauma, dehydration from vomiting or gastroenteritis, excessive exercise without carbohydrate replacement, or failure to adjust insulin during illness.
What should caregivers keep ready?
Caregivers should have the following:
- A written emergency plan with medication details
- A glucometer with extra strips and batteries
- Fast acting glucose (gel, tablets, or juice)
- Emergency contact numbers and medical ID
Where can I find more training or guidance?
You can enroll in CPR Select’s online First Aid training and certification, which covers diabetic emergencies and other critical situations with flexible, self paced learning. Certified programs from providers like the American Red Cross, St John Ambulance, and local health authorities are also available to help caregivers and bystanders respond effectively.