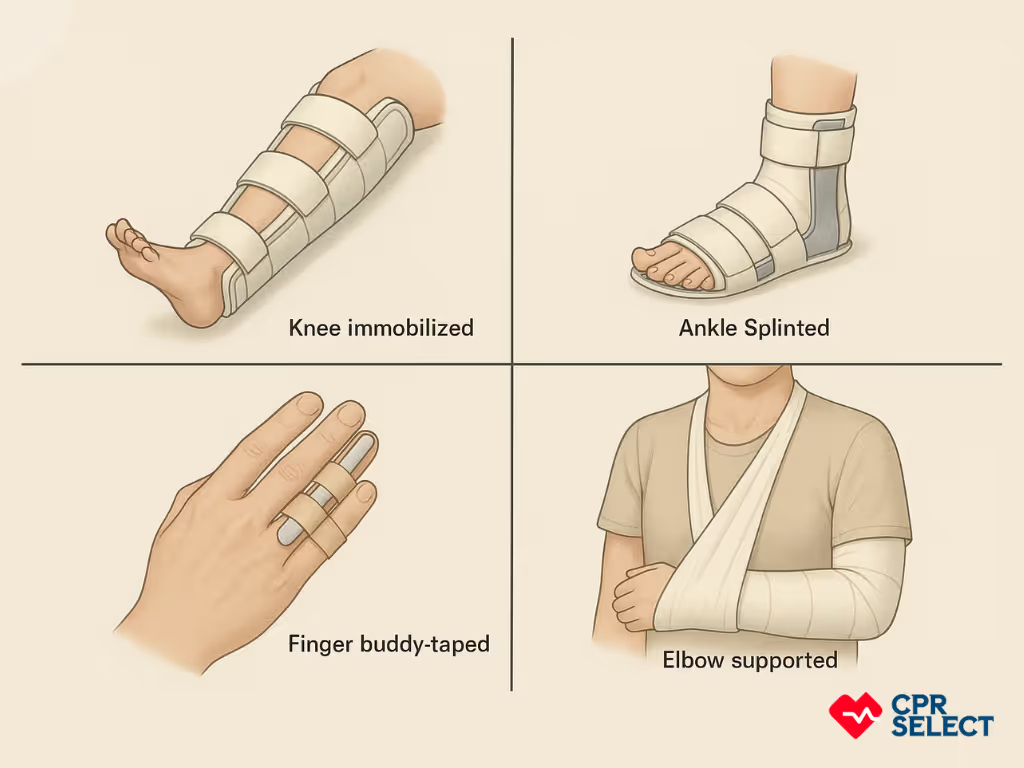
This article explains the importance of quick, informed care for joint dislocations and provides clear first aid steps. This guide helps lay responders, caregivers, first aiders, and sports coaches recognize dislocations. It shows them how to call emergency services, immobilize joints with slings or splints, and manage pain or shock. Readers will also learn common causes, signs, and differences between dislocations, fractures, and sprains, plus safe care for joints like the shoulder and fingers. The goal is simple: give anyone practical guidance to prevent further damage until professional treatment is available.
What Are Dislocations?
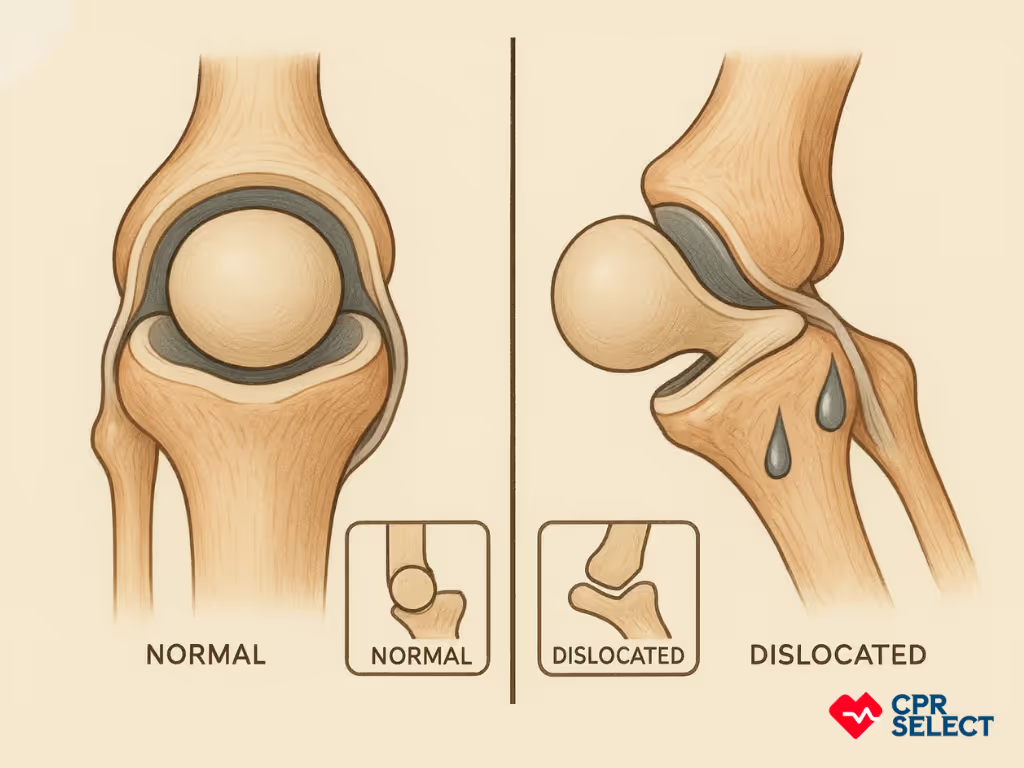
A dislocation is a joint injury where bones move out of their normal position, causing deformity, pain, and loss of function. It happens when the stabilizing structures (ligaments, joint capsule, or muscles) fail under force. This makes it different from a sprain or strain.
They are usually caused by trauma such as falls, blows, or twists. Examples include falling on an outstretched hand (shoulder dislocation), a blow to a bent knee (patellar or knee dislocation), or twisting under load (finger or thumb dislocation). Repetitive stress or weak connective tissues, like in Ehlers–Danlos syndrome, can also increase risk.
Which joints are most commonly dislocated?
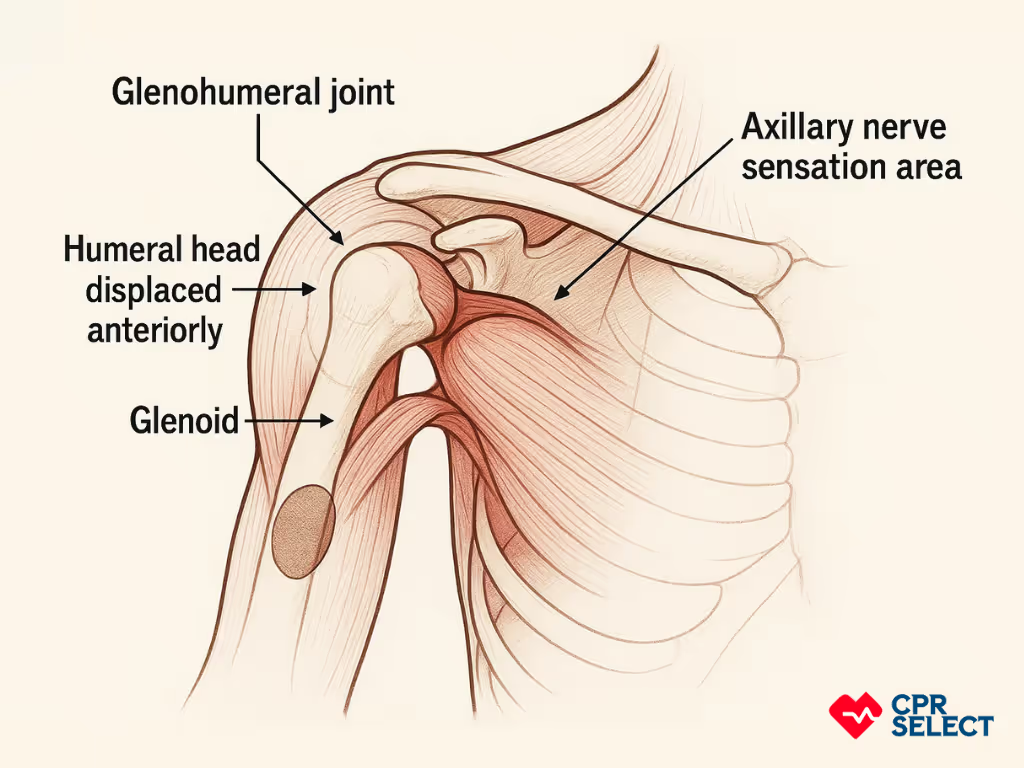
The shoulder is the most frequently dislocated joint, usually displaced forward. Fingers, thumbs, and elbows are also common due to their mobility. In the lower body, the hip and knee can dislocate, though less often. These injuries are particularly serious: hip dislocations can compromise blood flow to the femoral head, and knee dislocations may damage the popliteal artery, as noted by the American Academy of Orthopaedic Surgeons.
Why is understanding dislocations important?
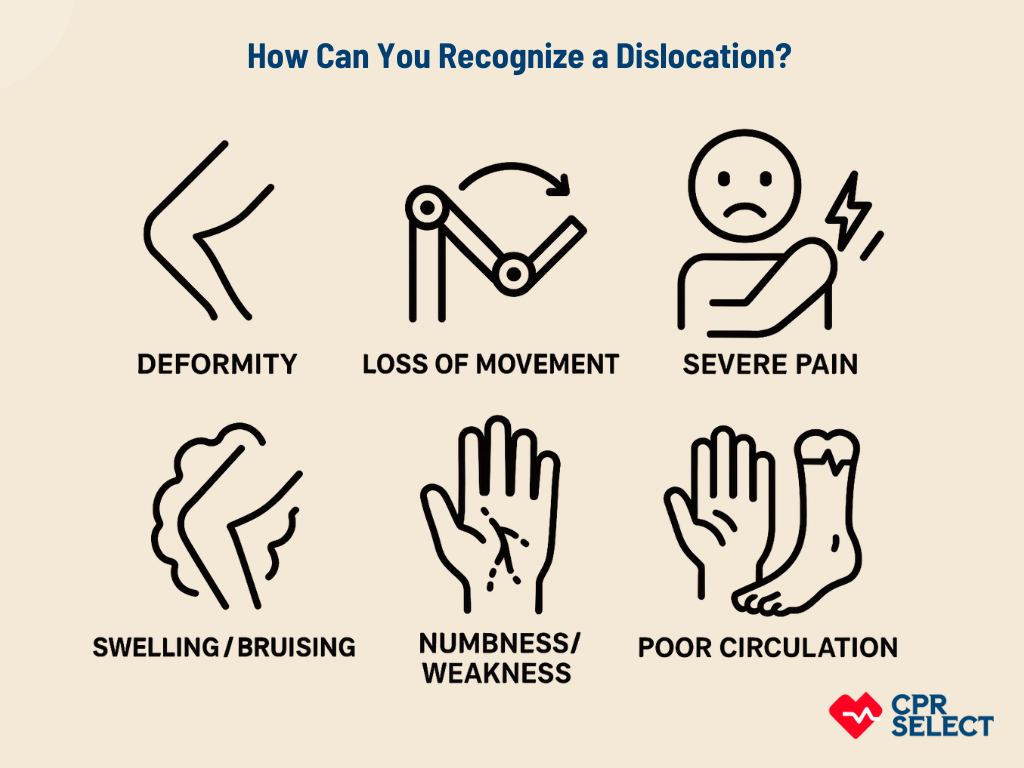
Recognizing dislocations quickly helps people give correct first aid. It also helps them communicate clearly with emergency responders. Key signs include visible deformity, severe movement limitation, and intense pain. While imaging confirms the diagnosis, early recognition guides safe first aid.
What Causes a Joint to Dislocate?
A joint dislocates when an external force overwhelms its stabilizing structures. This often happens during high-impact events such as sports collisions, falls, or motor vehicle accidents.
What mechanical forces can cause a dislocation?
Dislocations occur when specific forces push a joint beyond its normal limits, damaging ligaments, capsules, or cartilage. The main types of forces include:
- Translational force: Pushes one bone straight out of alignment, tearing ligaments or the joint capsule (e.g., anterior shoulder dislocation).
- Torsional force (twisting): Rotates the joint, damaging cartilage and ligaments (e.g., twisting knee injury).
- Hyperextension: Forces the joint past its normal range, often causing tendon and capsule damage (e.g., elbow dislocation).
What situations commonly cause dislocations?
Certain scenarios make these forces more likely. These include:
- Sports injuries: High-velocity tackles or impacts can rupture ligaments and dislocate joints, especially the shoulder.
- Falls: Landing on an outstretched limb or direct impact can force joints out of place.
- Accidents: Vehicle crashes or industrial injuries apply combined forces that may cause both dislocations and fractures.
- Direct blows: A focused hit can knock bones out of alignment (e.g., radial head dislocation in the elbow).
- Repetitive stress: Ongoing microtrauma weakens ligaments, making joints prone to future dislocations (e.g., chronic shoulder instability).
All these causes share sudden force, abnormal motion, or weakened support structures, which lead to loss of alignment. These same forces also produce visible signs and symptoms, which will be discussed in the next sections.


.avif)
.avif)