Eye injuries are damage to the eyeball or periocular tissues that can impair visual acuity and cause ocular pain, periocular bleeding, or ocular infection. Timely first aid is critical. Prompt action can preserve sight and prevent serious complications. This guide equips you with practical skills for recognizing common eye injuries, delivering immediate care, and knowing when urgent ophthalmology referral is needed. Whether you’re a family caregiver, safety officer, or first responder, you’ll learn step-by-step protocols, prevention strategies, and clear decision points.
.avif)
What are the Different Types of Eye Injuries
Eye injuries can be grouped by the cause of damage and the structures affected. Recognizing the category is vital for first aid, triage, imaging, and predicting visual outcomes.
1. Blunt trauma
Nonpenetrating force to the eyeball or orbital bones, such as from a ball strike or a punch. Signs include eyelid swelling, bruising, pain, and reduced vision. Check pupil size and reaction; a fixed or irregular pupil may indicate serious damage. Look for blood in the front of the eye (hyphema) with the patient upright. Prompt CT imaging and urgent ophthalmology referral are often needed.
.avif)
2. Penetrating injury
A full-thickness laceration of the cornea or sclera from sharp objects like metal shards or glass. Signs include visible cuts, fluid leakage, or protruding tissue. Never press on the eye; shield it instead. A teardrop-shaped pupil or tissue extrusion signals an open globe, which requires immediate surgical repair.
3. Chemical burn
Damage from acids or alkalis in substances like cleaning agents. Symptoms include severe pain, redness, cloudy cornea, and vision loss. Irrigate immediately with clean water or saline until pH is neutral, checking with pH paper. Alkali burns require longer flushing because they penetrate deeper.
4. Intraocular foreign body
Objects lodged inside the eye after trauma, such as metal fragments from grinding or wood splinters. May cause sudden vision loss, bleeding inside the eye, or a firm, hard globe. CT scans confirm metallic or glass objects; ultrasound is safe only if no open globe is present. Surgery is usually required to prevent infection or retinal damage.
Understanding these categories clarifies how to recognise and respond to specific ocular emergencies. The next section on Signs and Symptoms of an Eye Injury will describe the clinical features that help match a presenting case to the injury categories above.
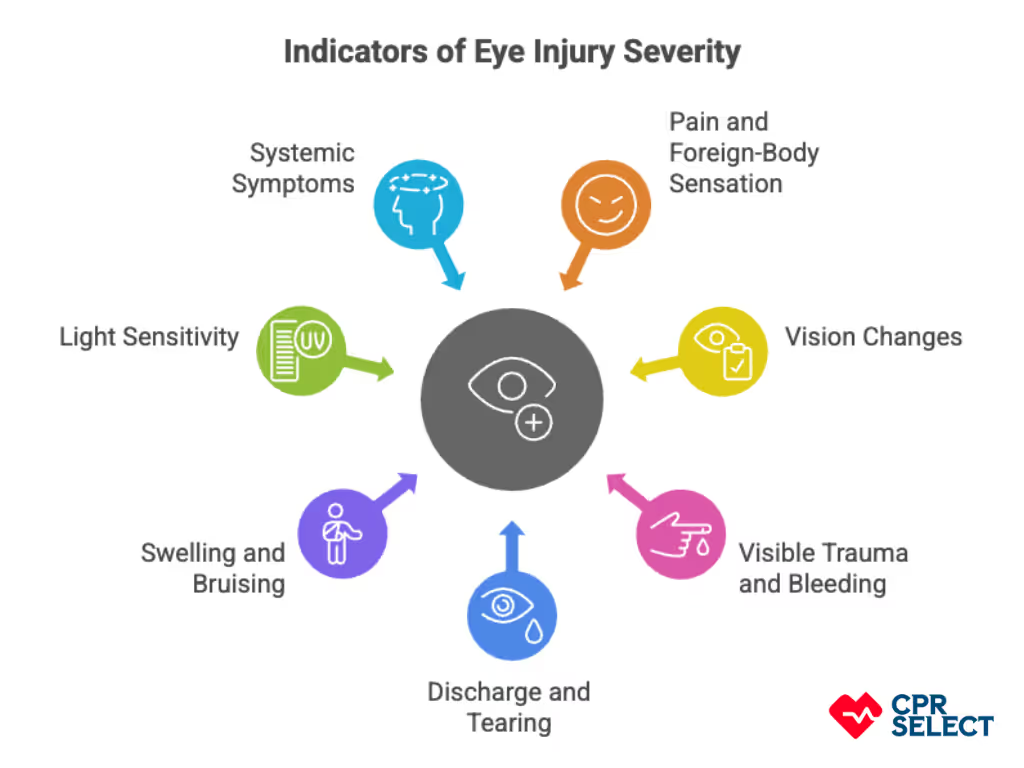
What are the Signs and Symptoms of an Eye Injury
Eye injuries show up through a mix of sensory changes, visible damage, loss of function, and whole-body reactions. Recognizing these patterns helps determine how urgent the situation is.
- Pain and foreign-body sensation: Sharp, burning, aching, or gritty feelings after trauma or chemical exposure. Pain that worsens with movement or comes with blurred vision may indicate corneal abrasion, penetrating trauma, or dangerous pressure changes in the eye.
- Vision changes: Blurred or double vision, partial vision loss, or sudden blindness can point to retinal detachment, globe rupture, or optic nerve injury. New floaters, flashes of light, or a curtain over the vision are red flags for retinal detachment.
- Visible trauma and bleeding: Cuts, tears, bruising, or pooling blood around the eye indicate direct structural injury. A peaked or misshapen pupil or tissue protrusion suggests a globe rupture—shield the eye immediately and seek urgent ophthalmology care.
- Discharge and tearing: Watery, mucoid, or pus-like discharge may signal infection, chemical irritation, or surface injury. Watery tearing is common after abrasions or chemical burns; pus usually suggests infection.
- Swelling and bruising: Puffy eyelids and discolored skin often follow blunt impacts. If swelling limits eye movement or causes double vision, an orbital fracture should be suspected and imaging may be needed.
- Light sensitivity (photophobia): Pain or squinting in bright light often follows corneal abrasion, uveitis, or chemical injury. Severe light sensitivity with an irregular pupil may mean deeper eye inflammation.
- Systemic symptoms: Nausea, vomiting, or fainting after eye trauma can signal serious injury like orbital compartment syndrome and require urgent hospital care.
Observing the signs and symptoms described improves diagnostic accuracy and determines the urgency and type of immediate action; the next section, First Aid for Eye Injuries, explains how recognizing the listed signs guides appropriate on-scene care and referral.




