Fainting, also called syncope, happens when blood flow to the brain drops and causes a brief loss of consciousness. Most episodes last less than two minutes and improve once the person lies flat, according to the Cleveland Clinic. Knowing how to recognize the warning signs and provide first aid is important to keep the person safe and prevent further injury. This guide explains the causes, symptoms, and the right steps to take if someone faints.
What is Fainting?
Fainting, or syncope, is a brief loss of consciousness caused by a temporary drop in blood flow to the brain. It usually happens suddenly, lasts only a few seconds to minutes, and often improves once the person is lying flat.
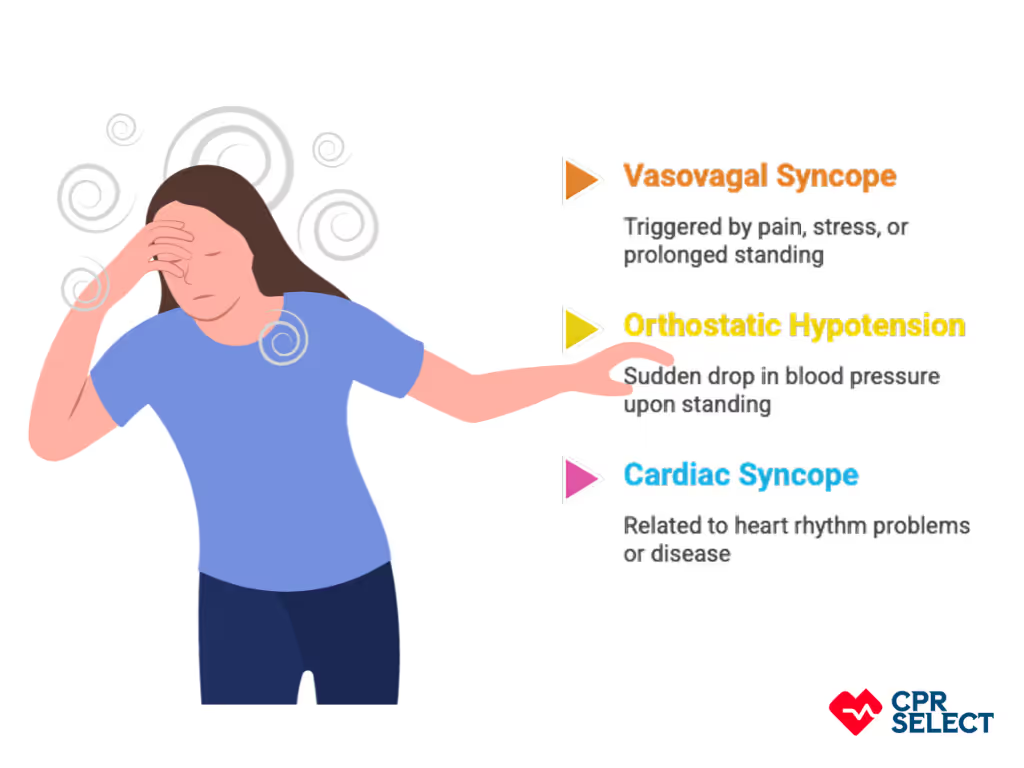
The most common causes include:
- Vasovagal syncope – triggered by pain, emotional stress, or standing too long.
- Orthostatic hypotension – a sudden drop in blood pressure when standing up, often linked to dehydration or medication.
- Cardiac syncope – related to heart rhythm problems or structural heart disease and requires urgent medical attention.
Before fainting, people may feel lightheaded, sweaty, or nauseated. First aid focuses on laying the person flat, elevating the legs if safe, and checking breathing and pulse. Call emergency services if the person doesn’t wake quickly or has chest pain, palpitations, or a known heart condition.
How Fainting Differs From a Seizure?
A seizure involves abnormal brain activity, often with jerking movements, tongue biting, or confusion afterward. Fainting, by contrast, usually has a quick recovery once blood flow returns to the brain.
How Fainting Differs From Hypoglycemia?
Low blood sugar causes weakness, shakiness, and sweating, but it does not resolve quickly by simply lying down. Unlike fainting, it requires food, glucose tablets, or medical care to restore sugar levels.
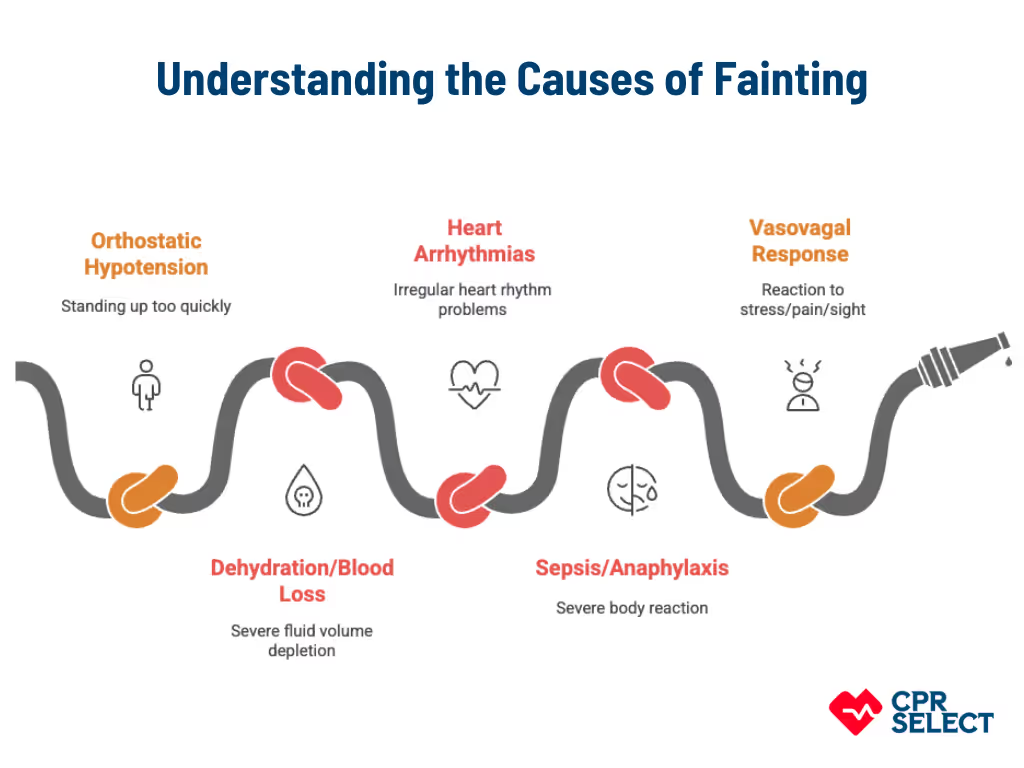
What Causes Fainting?
Fainting happens when blood or oxygen flow to the brain drops, leading to a short loss of consciousness. Common causes of fainting include:
- Standing up too quickly (orthostatic hypotension)
- Severe dehydration or blood loss
- Irregular heart rhythms (arrhythmias)
- Sepsis or severe allergic reaction (anaphylaxis)
- Vasovagal response to pain, stress, or the sight of blood
- Pressure on the neck (carotid sinus sensitivity)
- Emotional distress or fear
- Intense coughing, sneezing, or straining
- Low blood sugar (hypoglycemia)
- Alcohol intoxication
- Side effects of medications (antihypertensives, diuretics, antiarrhythmics)
- Heat exposure or prolonged standing
- Intense physical exertion
Multiple grouped mechanisms can cause fainting, and identifying the likely trigger helps guide immediate response and further diagnostic evaluation.
What are the Symptoms Before Fainting?
Before fainting, people often experience warning signs caused by reduced blood flow to the brain. Common symptoms include:
- Lightheadedness or dizziness – often worse when standing
- Heart palpitations or chest pressure – may signal arrhythmia or other heart issues
- Blurred or tunnel vision – eyesight narrows or becomes unclear
- Confusion or slowed thinking – brief disorientation before collapse
- Sweating, nausea, or clammy skin – common in vasovagal fainting
- Pale skin – due to reduced blood flow
- Sudden fatigue or weakness – feeling drained or unable to continue activity
- Loss of balance or stumbling – often the last sign before fainting
These symptoms can appear alone or in clusters. Recognizing them early helps prevent falls and guides when to apply first aid or call for emergency help.
How to Provide First Aid for a Fainted Person
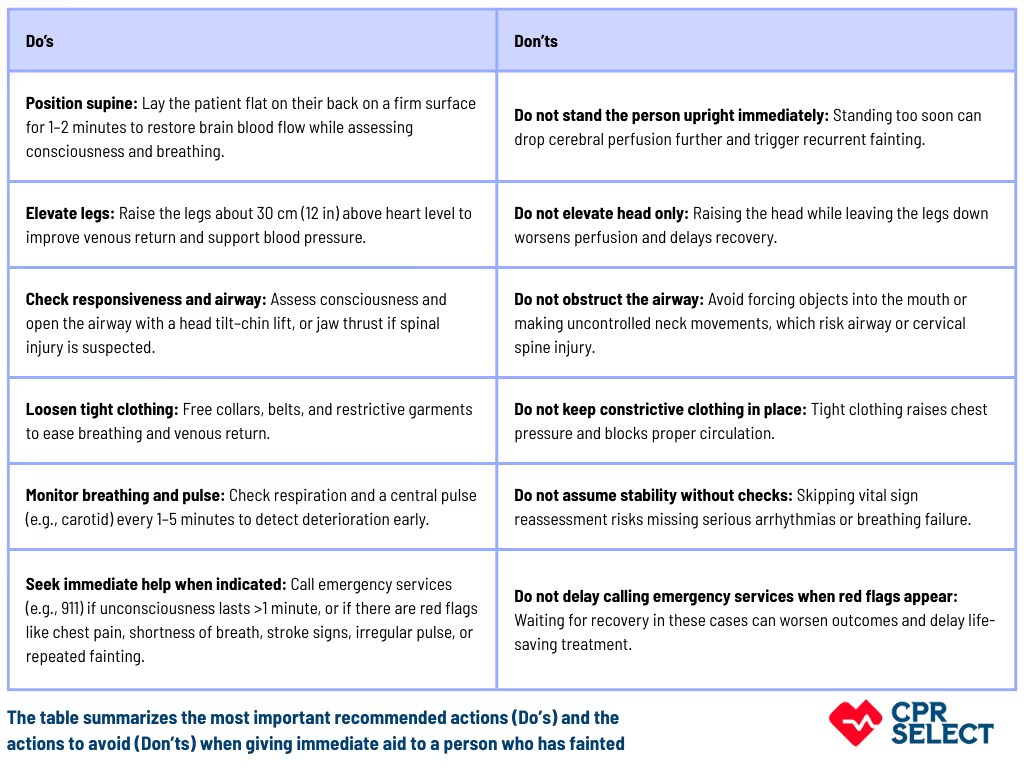
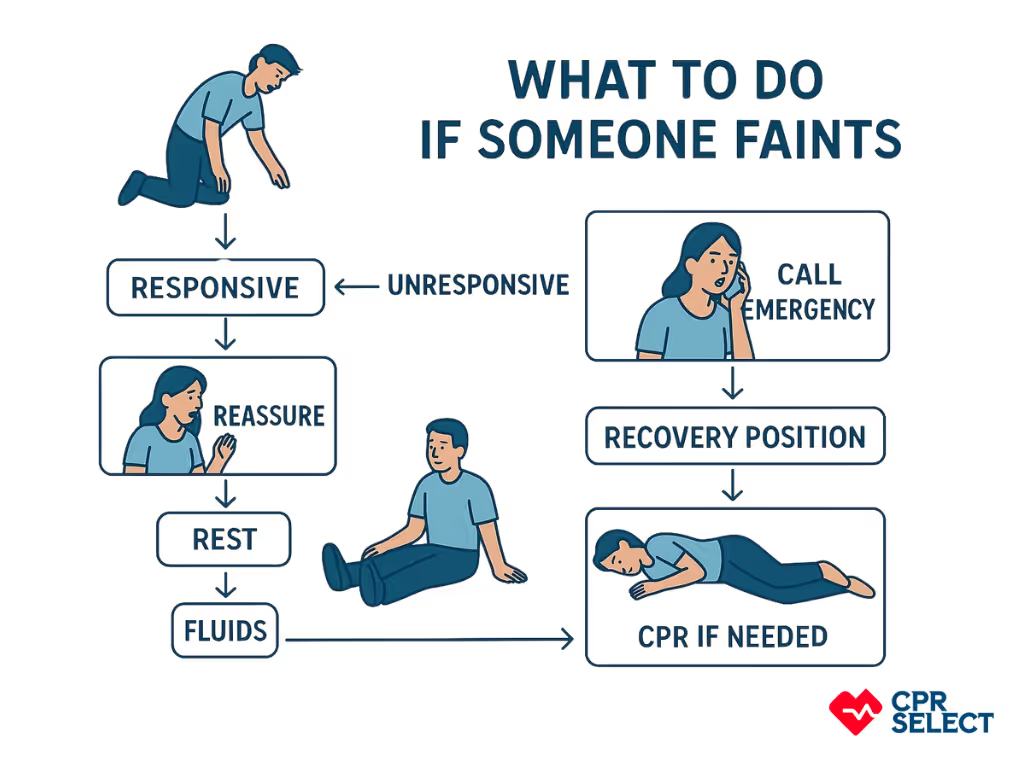
First aid for fainting focuses on safety, airway, circulation, and timely escalation. The steps below outline how to stabilize someone, restore blood flow, and prevent complications.
- Ensure scene safety – Check for hazards (traffic, wires, chemicals). Remove the person only if danger remains. If unsafe, have a bystander call emergency services.
- Check responsiveness – Speak loudly, tap the shoulder, and look for signs of consciousness. If unsure, call for help immediately.
- Call for help if unresponsive or injured – If no response or trauma is suspected, activate emergency services. If unresponsive but breathing, place in recovery position. If not breathing or abnormal, start CPR and use an AED if available.
- Position safely – Place a breathing but unconscious person in the recovery position (side, head slightly back, airway clear). If assessing circulation, keep flat on their back. Elevate legs ~30 cm to improve blood flow unless injury (hip, pelvis, spine, or legs) is suspected.
- Open airway and check breathing – Use head tilt–chin lift; if spinal injury suspected, use jaw thrust. Look, listen, and feel for normal breathing for 10 seconds. Begin CPR if absent or abnormal.
- Loosen restrictive clothing and manage temperature – Remove tight garments at neck, chest, and waist. If overheated, cool with a damp towel (~20–25°C). If cold, cover with a blanket. Avoid sudden temperature changes. Do not give food or fluids until fully alert.
- Monitor vital signs and consciousness – Track pulse, breathing, skin color, and alertness every 1–5 minutes. Watch for apnea, bradycardia, weak pulses, or pallor. If no reliable pulse and no breathing, start CPR.
- Assist recovery – If the person regains consciousness, reassure them. Keep supine 5–10 minutes before slowly helping them sit up. Offer fluids if fully alert and no nausea. Recommend medical review within 24–48 hours if cause is unclear.
- Document and hand over – Record time of collapse, symptoms before fainting (lightheadedness, nausea, vision changes, palpitations), first aid given, vital signs, and medical history. Share with paramedics for continuity of care.
Clear, sequential first aid actions stabilize most uncomplicated fainting episodes, while specific clinical contexts require modified interventions.


.avif)