Hyperglycemia occurs when the body has too much glucose in the blood, often due to problems with insulin production or use. This article explains what hyperglycemia is, its common causes, warning signs, and possible complications. It also highlights why understanding first aid for hyperglycemia is important and how enrolling in CPR Select’s online First Aid Training can help you respond effectively during a diabetic emergency.
What is Hyperglycemia?
Hyperglycemia, or high blood sugar, is a condition where there is too much glucose in the blood due to impaired insulin production or action. It is common in people with diabetes and serves as a key indicator of poor blood sugar control.
The condition occurs when glucose builds up in the bloodstream because the body cannot use insulin properly or produce enough of it. This imbalance can result from reduced insulin secretion, insulin resistance, or increased glucose production by the liver.
What are the Causes of Hyperglycemia?
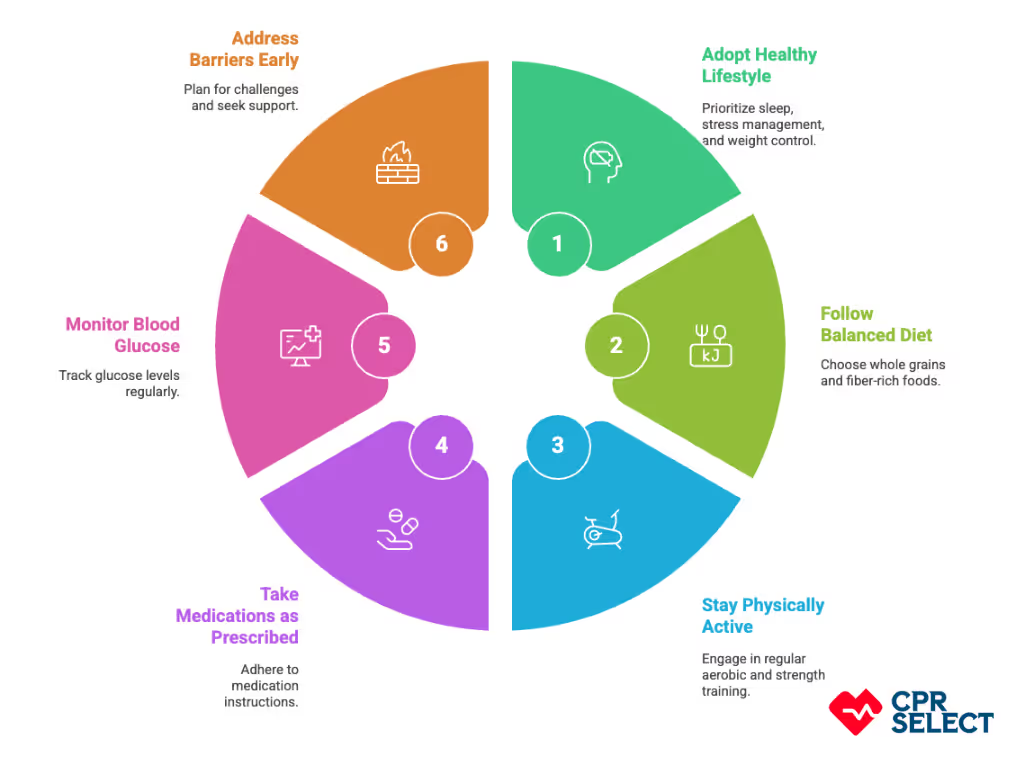
Hyperglycemia happens when blood sugar levels rise because the body can’t use insulin properly or too much glucose enters the bloodstream. The causes generally fall into three main categories: lifestyle, medical, and situational factors.
1. Lifestyle Factors
Everyday habits can raise blood sugar by increasing glucose intake or reducing insulin effectiveness. Common examples include eating too many high-sugar foods, lack of physical activity, and missing or mistiming insulin or oral medications. These causes are often preventable through healthier routines and better treatment adherence.
2. Medical Factors
Health conditions and certain treatments can disrupt blood sugar control. These include diabetes, pancreatic disorders, hormonal conditions like Cushing’s syndrome, and medications such as steroids or antipsychotics. Unlike lifestyle causes, these are linked to physiological or treatment-related issues.
3. Situational Triggers
Temporary events like infections, surgery, trauma, or severe stress can trigger spikes in blood glucose. These situations cause hormonal and inflammatory responses that increase glucose production and reduce its use in cells.
Often, multiple factors combine, such as illness plus missed medication, leading to more severe and prolonged hyperglycemia. Understanding how these causes interact helps prevent complications like diabetic ketoacidosis or hyperosmolar hyperglycemic state.
What are the Symptoms of Hyperglycemia?
Hyperglycemia shows several warning signs that vary in severity. These symptoms can be grouped into mild, moderate, and severe categories based on how much they affect daily function and health.
- Mild Symptoms: Increased thirst, frequent urination, mild fatigue, and occasional blurred vision after meals.
- Moderate Symptoms: As blood sugar rises, symptoms become more noticeable: frequent nighttime urination, extreme thirst, significant fatigue, unexplained weight loss, and persistent blurred vision.
- Severe Symptoms: Deep, rapid breathing, confusion, vomiting, abdominal pain, and fainting may appear. These can signal emergencies like diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS) and require immediate medical care.
Recognizing symptoms early helps prevent dangerous complications. Continuous glucose monitoring and awareness of these signs support timely action and better blood sugar management.

What Are the Complications of Untreated Hyperglycemia?
If left untreated, hyperglycemia can lead to serious short-term emergencies and long-term organ damage. The two major acute conditions are diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS), while chronic effects include microvascular and macrovascular complications.
What Happens During Acute Metabolic Emergencies?
- Diabetic Ketoacidosis (DKA): Caused by severe insulin deficiency, leading to high ketone levels, acidosis, dehydration, and rapid breathing. It develops quickly and requires emergency care.
- Hyperosmolar Hyperglycemic State (HHS): Results from extreme blood sugar levels, causing severe dehydration and confusion. It develops over several days and can be life-threatening without prompt treatment.
-
What Are the Early Systemic Effects?
Before these emergencies occur, dehydration, electrolyte imbalances, and increased infection risk may develop. Prolonged high blood sugar weakens the immune system and disrupts fluid balance, setting the stage for serious complications.
What Are the Long-Term Complications?
Long-term hyperglycemia damages blood vessels and nerves:
- Microvascular damage: leads to eye (retinopathy), kidney (nephropathy), and nerve (neuropathy) problems.
- Macrovascular damage: increases the risk of heart attack, stroke, and peripheral artery disease.
How Does It Affect Daily Life?
Chronic complications can cause vision loss, limited mobility, chronic pain, and kidney failure requiring dialysis. They greatly reduce quality of life and increase healthcare needs.
Who Is at Higher Risk for Complications?
Factors that worsen complications include uncontrolled blood sugar (high HbA1c), long disease duration, hypertension, obesity, smoking, and poor access to treatment.
What’s the Difference Between Hyperglycemia and Hypoglycemia?
Hyperglycemia vs. hypoglycemia compares high blood sugar to low blood sugar. The key difference is that hyperglycemia requires safely lowering excess glucose, while hypoglycemia needs fast glucose replacement to prevent brain complications. Knowing the difference helps guide the right first aid response: hydration and medical care for high blood sugar, and rapid glucose intake for low blood sugar.
The comparison below highlights the distinct causes, symptoms, and first-aid steps for each condition:

Why Do Causes Matter?
Causes determine how urgent the response should be. Hyperglycemia often results from missed insulin or illness, guiding first aid toward hydration and medical assessment. Hypoglycemia, on the other hand, stems from too much insulin or skipped meals, requiring immediate glucose intake.
How Can You Tell the Difference Through Symptoms?
Look for quick clues. Hypoglycemia often causes sweating, tremors, confusion, or pale, clammy skin. Hyperglycemia causes warm, dry skin, excessive thirst, frequent urination, fruity-smelling breath, and deep breathing. Recognizing these differences in hyperglycemia vs. hypoglycemia helps responders act fast and appropriately.
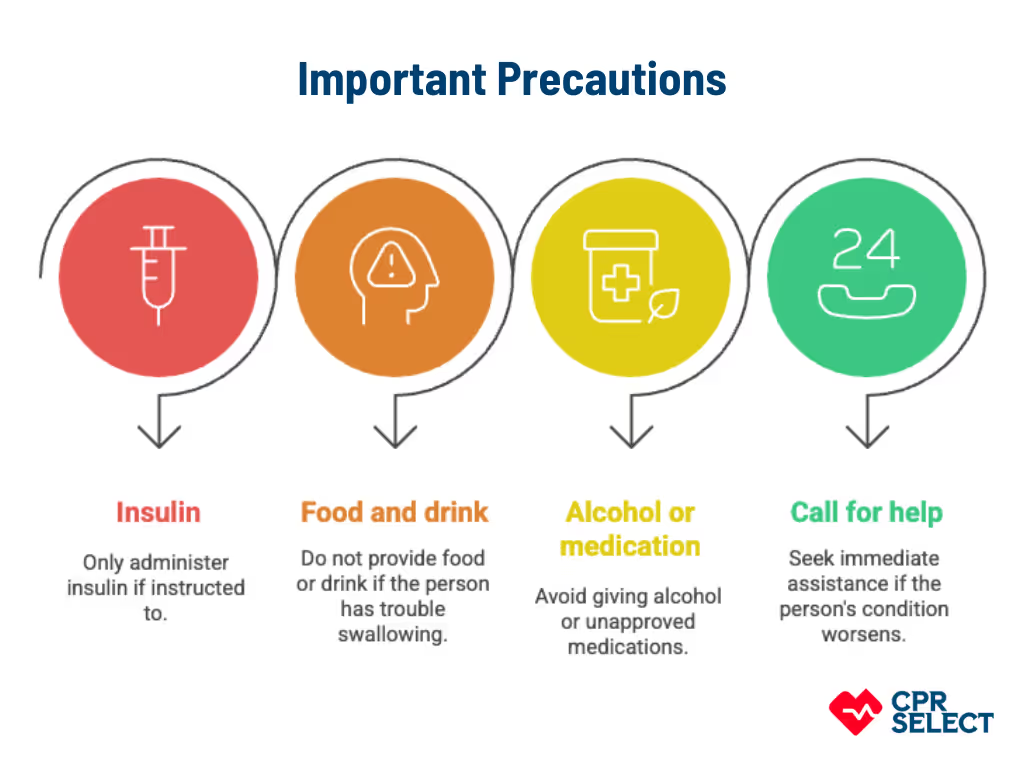
What Are the First Aid Priorities?
For hypoglycemia, if the person is conscious, give 15–20 grams of fast-acting carbohydrates and recheck blood sugar after 10–15 minutes.
For hyperglycemia, focus on oral hydration, watching for dehydration or diabetic ketoacidosis, and seeking urgent medical care.
If the person becomes unconscious, call emergency services immediately.
What If Symptoms Overlap?
Sometimes signs can be unclear. If in doubt, prioritize safety: check responsiveness, maintain an open airway, and call for medical help. It’s safer to treat for possible hypoglycemia first if severe confusion or unresponsiveness is present.