Hypoglycemia, or low blood sugar, occurs when blood glucose levels drop below the normal range, usually under 70 mg/dL. It can happen suddenly and become life-threatening if not treated quickly. This article explains the signs and symptoms of hypoglycemia, what to do during an episode, and how CPR Select’s Online First Aid Training can help you respond confidently and effectively in emergencies.
What Is Hypoglycemia?
Hypoglycemia refers to an abnormally low level of glucose in the blood that deprives the body, especially the brain, of its main energy source. This condition can quickly cause symptoms such as sweating, trembling, confusion, blurred vision, or, in severe cases, seizures and loss of consciousness.
Normal blood glucose levels typically stay above 70 mg/dL (3.9 mmol/L). Readings below this threshold signal possible hypoglycemia, while levels under 54 mg/dL (3.0 mmol/L) are considered clinically significant and require immediate action, according to the American Diabetes Association and International Hypoglycaemia Study Group.
Recognizing and treating hypoglycemia promptly is critical to prevent serious complications. The next section explores the main triggers and underlying mechanisms of low blood sugar.
What Causes Hypoglycemia?
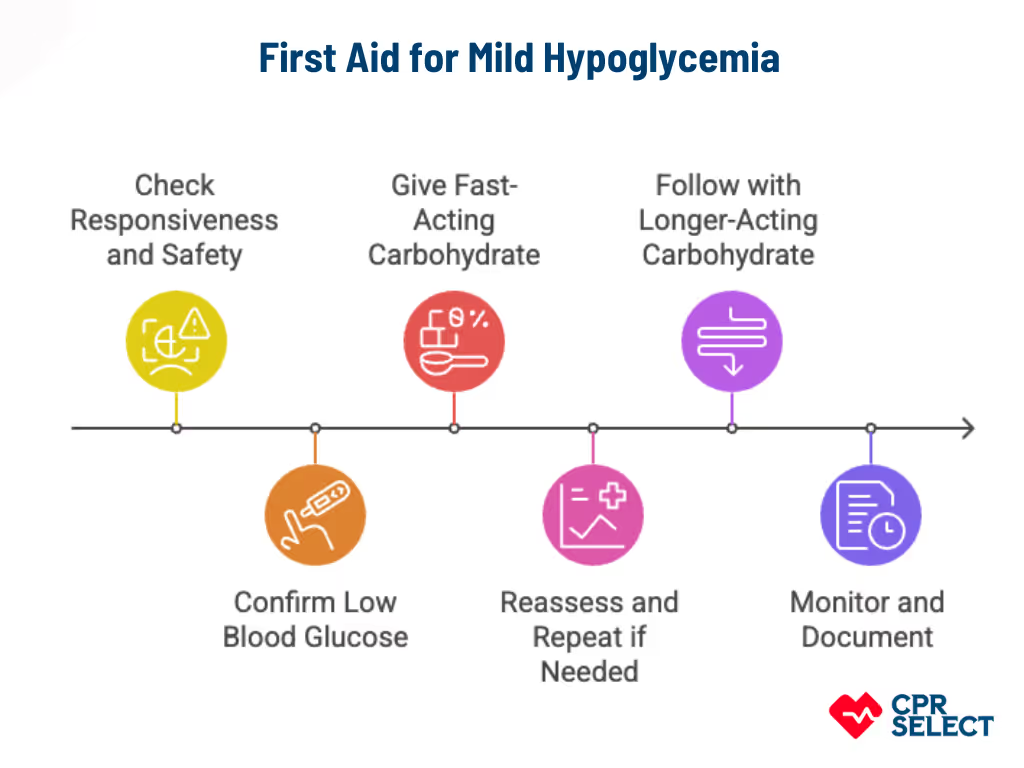
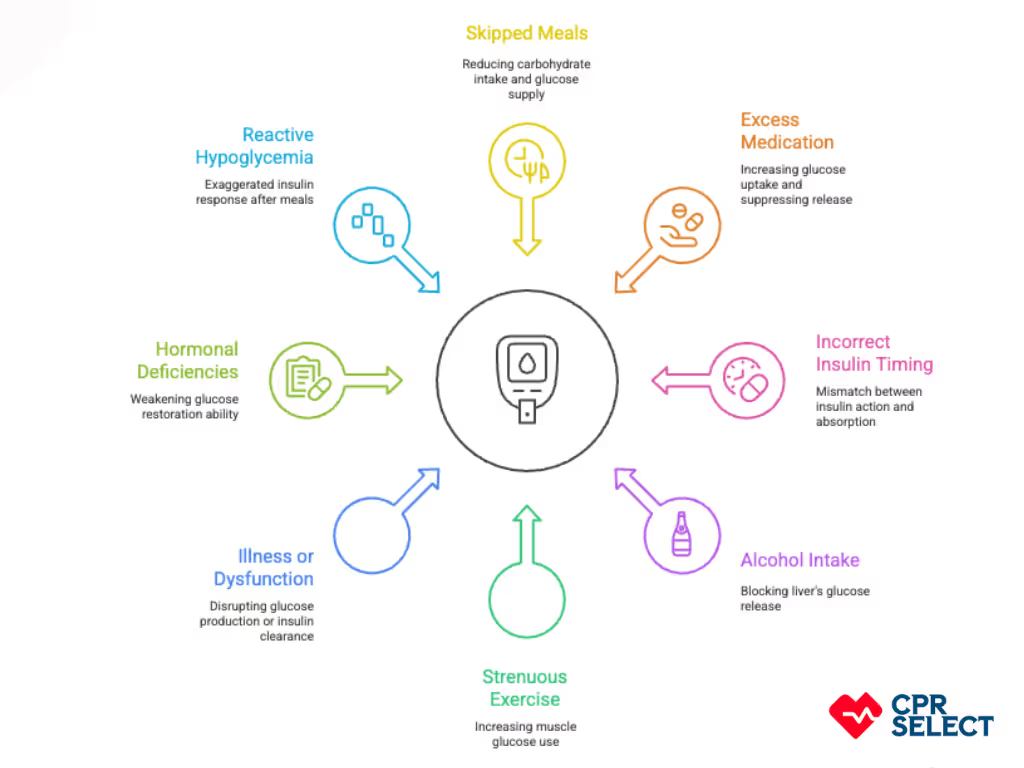
Hypoglycemia occurs when blood glucose drops below normal levels, and several common causes can lead to this condition. The list below outlines frequent causes with brief explanations showing how each one lowers blood glucose or increases the body’s glucose demand.
- Skipped meals: Missing or delaying meals reduces carbohydrate intake and glucose supply in the bloodstream. This directly leads to low blood sugar, especially in people taking insulin or sulfonylureas, as liver glycogen stores become depleted within 12 to 24 hours.
- Excess diabetes medication: Taking more insulin or insulin secretagogues than needed increases glucose uptake by cells and suppresses glucose release from the liver. This imbalance commonly leads to severe hypoglycemia, as noted in clinical diabetes guidelines.
- Incorrect insulin timing: Giving insulin too early, too late, or in excessive doses causes a mismatch between insulin action and carbohydrate absorption. This timing error results in blood glucose dropping after the insulin peak.
- Alcohol intake: Drinking alcohol, especially on an empty stomach, blocks the liver’s ability to release glucose. Alcohol metabolism interferes with enzymes responsible for gluconeogenesis, leading to low blood sugar.
- Strenuous exercise: Intense or prolonged physical activity increases muscle glucose use. Without adequate carbohydrate intake or medication adjustments, glucose levels can drop, and insulin sensitivity may remain elevated for several hours afterward.
- Illness or organ dysfunction: Conditions such as liver failure, kidney disease, or endocrine disorders can disrupt glucose production or insulin clearance. These impairments raise the risk of hypoglycemia, as the body cannot maintain normal glucose levels.
- Hormonal deficiencies: A lack of key hormones like glucagon, cortisol, or growth hormone weakens the body’s ability to restore glucose levels. Disorders such as adrenal insufficiency and pituitary dysfunction often lead to recurring low blood sugar.
- Reactive hypoglycemia: Some people experience an exaggerated insulin response after meals, causing glucose to fall several hours later. This pattern is confirmed through tests such as a mixed-meal or oral glucose tolerance test.
Hypoglycemia often results from multiple overlapping factors, and identifying the exact cause is essential for proper first aid and prevention. The next section will describe how these causes translate into observable signs and symptoms.
What Are the Symptoms of Hypoglycemia?
Symptoms of hypoglycemia appear in stages: mild, moderate, and severe. Recognizing these stages helps provide quick and appropriate first aid to prevent complications.
The table below groups signs by severity for easy reference. It is designed for recognition and not as a treatment guide.

Hypoglycemia symptoms progress from mild to severe. Early signs like tremor, sweating, anxiety, and hunger are warning cues that blood sugar is dropping. As levels fall further, confusion, slurred speech, blurred vision, and poor coordination may appear. In severe cases, hypoglycemia can cause seizures, loss of consciousness, or breathing difficulties, requiring immediate medical attention.
Symptoms may vary depending on age, medications, and overall health. They may not always appear in order.